How to Cite | Publication History | PlumX Article Matrix
Samarpita Mukherjee1 , Shubhrajit Saha2*
, Shubhrajit Saha2* , Ushasi Banerjee3
, Ushasi Banerjee3 , Arup Kumar Banerjee3
, Arup Kumar Banerjee3 and Ritam Banerjee2
and Ritam Banerjee2
1Institution Woodland Multi-Speciality Hospital. 17/7, Priyanath Ghosh Street, Belgharia, Kolkata: 700056. West Bengal,India.
2Department of Biochemistry Institution Maharaja Jitendra Narayan Medical College And Hospital, Coochbehar, West Bengal, India.
3Department of Biochemistry, Institution North Bengal Medical College And Hospital. Sushrutanagar, P.O Thiknikata, Darjeeling. Pin: 734012
Corresponding Author Email: shubhrajit87@gmail.com
DOI : http://dx.doi.org/10.13005/bbra/2876
ABSTRACT: Background and Objectives In the last few decades,Nonalcoholic Fatty Liver Disease (NAFLD) has become a common health issue that leads to serious complications like cirrhosis, cardiovascular disease, etc. Insulin resistance (IR) is the key pathogenic factor for NAFLD. The young medicos being habituated in stressful and sedentary lifestyle and representative of the youth as well can fully justify their selection as study population and help to build social awareness by emphasizing the importance of early lifestyle modifications in preventing or delaying the severe complications of NAFLD. This study is aiming to find out if there is any correlation of hepatic steatosis with IR, Alanine Transaminases (ALT), Aspartate Transaminases (AST) or Gama Glutamyl Transferases (GGT) and also to identify if one enzyme is better correlating with hepatic steatosis than others in the scenario of Insulin Resistance among young medicos. METHODS: 132 medical students of North Bengal Medical College, aged between 18-25 years were included in this institution based observational cross-sectional study. Their Fasting Insulin, glucose, ALT, AST, GGT were measured, and IR was calculated by the Homeostatic Assessment of Insulin Resistance (HOMA-IR) calculator. Sonography was done to assess Hepatic steatosis. RESULTS: Among 132 subjects normal, grade 1 and grade 2 fatty changes have been found in 67.4%, 25%, and 7.6% of the study population respectively. The Grouping was done using the cut-off value of IR (i.e. subjects with IR<1.525 vs. IR≥1.525). Significant differences were found in the mean values of ALT, AST, GGT between groups. Significant positive concordances were found between enzymes ALT, GGT, and hepatic steatosis in subjects having IR ≥ 1.525.Regression analysis showed that higher GGT values have a stronger positive correlation with hepatic steatosis than ALT among the same. Interpretation and Conclusion From this study, we can interpret that subjects having higher GGT values are better associated with steatosis than those having higher ALT values and can lead us to the conclusion that GGT might be an important independent marker for NAFLD associated with IR. Furthermore, such observations may suggest considering GGT as a marker for assessing the severity of fatty liver irrespective of etiopathogenesis, though the population-based vivid evaluation is highly recommended.
KEYWORDS: ALT; AST; GGT; Hepatic Steatosis; Insulin Resistance; Medicos; NAFLD
Download this article as:| Copy the following to cite this article: Mukherjee S, Saha S, Banerjee U, Banerjee A. K, Banerjee R. A Correlational Study of Hepatic Steatosis (Fatty Liver Disease) and Liver Enzymes (ALT, AST, GGT) In The Scenario of Insulin Resistance Among Young Medicos. Biosci Biotech Res Asia 2020;17(4). |
| Copy the following to cite this URL: Mukherjee S, Saha S, Banerjee U, Banerjee A. K, Banerjee R. A Correlational Study of Hepatic Steatosis (Fatty Liver Disease) and Liver Enzymes (ALT, AST, GGT) In The Scenario of Insulin Resistance Among Young Medicos. Biosci Biotech Res Asia 2020;17(4). Available from: https://bit.ly/2VTNntE |
Introduction
Nowadays Nonalcoholic fatty liver disease (NAFLD) has become an emerging health issue in adultsand children. It is a condition with similar histology with alcoholic liver disease but without any history of alcohol intake and the disease,the spectrum includes nonalcoholic fatty liver, nonalcoholic steatohepatitis, liver cirrhosis, and hepatocellular carcinoma1-3. In western countries, at least one-quarter of the general population is being affected by NAFLD. Adaptation of sedentary lifestyle like west and increasing frequency of obesity contributes to increased prevalence of NAFLD in the Asia-pacific region over the past two decades4,5and India is no exception to this scenario.6,7. Though it is more common in adults, now it is affecting children and young adults, especially obese ones1.
The pathogenesis of NAFLD has been proposed as a two-hit model by Day and James. The “first hit” takes place with the accumulation of lipids in the hepatocytes and insulin resistance is the main contributor to hepatic steatosis8-10.The “second hit” leads to hepatocyte injury, inflammation, and fibrosis. Oxidative stress and subsequent lipid peroxidation, pro-inflammatory cytokines, adipokines, and mitochondrial dysfunction are behind the “second hit”8.
NAFLD is often diagnosed after the finding of mildly abnormal LFTs. It happens to be the most common cause of elevated Transaminases other than viral and alcoholic hepatitis. However, liver Transaminase levels rarely reach beyond 3 or 4 times the upper normal limit. Serum Transaminases elevation is linked with higher body mass index, waist circumference, serum triglycerides, and fasting insulin, and lower HDL cholesterol1,11.The Alanine Transaminases (ALT) levels are higher than the Aspartate Transaminases (AST) levels in most instances1,12. It has also been found that Gamma-Glutamyl-Transferase (GGT) is elevated in persons having NAFLD13,14 and it is frequently associated with insulin resistance and higher BMI15,16.
In healthy individuals, some amount of cytoplasmic enzyme, like ALT, AST (within the reference range) are present in the circulation mainly due to cell leakage. In pathological conditions, Cell injury allows more leakage of cytoplasmic enzymes from cells, but a minimal release of other types of enzymes. Synthesis of GGT also increases in diseased human liver16.The mechanism of release of membrane-bound enzymes such as GGT into the circulation is less well understood. Elevated Serum GGT level probably reflects ongoing chronic inflammation; often associated with low levels of anti-inflammatory hormones e.g. adiponectin or with reduced effectiveness of insulin as a modulator of cytokine action.17,18 GGT is often found to be high in hepatic steatosis associated with insulin resistance presenting with chronic inflammation due to oxidative stress.17
The medicos who are nowadays habituated toa sedentary lifestyle are the population at risk because of the intense stress they go through before and after joining the curriculum. So they easily fall prey to metabolic derangement which has long-term adverse effects. But these harms can be prevented early, simply by changing lifestyle, regular exercise, weight reduction19,20. Justification for selecting young medicos lies in the fact that; as they are representing the medical fraternity as well as the youth, through their awareness about the risk factors of NAFLD, can be spread to society so that more severe complications developing from this can be avoided.
In this context, the present study is aiming to correlate hepatic steatosis with IR, ALT, AST, and GGT and to find out the Enzyme better correlating with hepatic steatosis than others in the Scenario of Insulin Resistance among young medicos of North Bengal Medical College and Hospital.
Materials and Methods
STUDY DESIGN: The present study is an institution-based observational study with a mixed design for a one-year duration.The study was conducted after approval from the Ethics committee of North Bengal Medical College and Hospital from April-2015 to March-2016 in the department of Biochemistry of North Bengal Medical College and hospital.
132 apparently healthy young medicos of North Bengal Medical College aged between 18-25 years were included in the study after detailed history taking. Informed consent was taken from all the subjects under the study.
Inclusion Criteria
AGE: 18-30 years
GENDER: both male and female.
Both under- graduate& post-graduate of North Bengal Medical College.
Apparently healthy individuals
Exclusion Criteria
Exclusion criteria for selection are the following Persons with a history of Habitual alcohol intake (Daily ingestion of less than 20 g ethanol has been suggested as the maximum alcohol intake compatible with a diagnosis of NAFLD) 16. Smoking, any other addiction or drug abuse like Cannabis, Opioids, Sedatives, etc. Any medication like lipid-lowering drugs, Paracetamol, Methotrexate, Barbiturates, Oral Contraceptives, Persons with any kind of liver, renal, or thyroid disorders, cardiovascular diseases (e.g. h/o Acute myocardial infarction, ischemic heart disease etc.), chronic obstructive pulmonary disease, pancreatic pathologies, gall bladder pathologies, febrile illness, Acute inflammatory conditions like Juvenile Rheumatoid Arthritis, Systemic Lupus Erythematosus, etc.
For all the subjects, thorough physical examinations including anthropometry were performed. Among laboratory investigations, fasting blood glucose and fasting insulin, liver enzymes were of paramount importance as per the study was concerned. 5-6 ml fasting blood sample was collected. Fasting blood glucose, ALT, AST were measured in an automated analyzer(Transasia- XL-600) using ERBA XL- system packs. GGT was measured in Transasia-CHEM 5X Semi-automated analyzer using reagents from (CORAL: Clinical systems).Insulin was assayed by the ELISA method using kits from Accubind in Robonik ELISA Washer and Reader. Quality assurance of the parameters under study was maintained by internal quality assurance. Insulin resistance was calculated with the help of the HOMA IR calculator. Ultrasonography was done for every case. Both subcostal and inter-costal scanning were done. Normal liver parenchyma is seen as solid homogenous echotexture which is midway between the renal cortex and pancreatic echogenicity. The findings of hepatic steatosis at sonography include increased echogenicity and sound attenuation.
Analysis of Data
The data obtained were analyzed by SPSS 20 software for Windows. Results obtained were arranged in tabular and graphical forms.
Cut off value of Insulin resistance in this study population is determined by ROC (receiver operating characteristics) curve using the same software. (State variables were: normal denoted by 0 and NAFLD group denoted by 1). The area under the ROC curve ranges from 0.5 to1.
The area under the curve 1 suggests a perfect test, 0.9-0.99 is an excellent one, 0.8-0.89 suggests a good test, 0.7-0.79 is fair test, 0.51-0.69 suggests poor one and <0.5 is a worthless test. Cut off value of IR was determined by fitting the highest value of sensitivity with the lowest value of 1- specificity. (Vide figure-1)
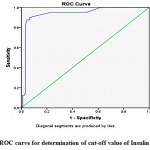 |
Figure 1: ROC curve for determination of cut-off value of Insulin Resistance. |
Results And Analysis
The study population consisted of 132 medicos aged between 18 to 25 years of North Bengal Medical College. A sample size of 122 was estimated taking prevalence as 10 percent, with 95 percent level of confidence using modified Cochran formula. We have screened all the medicos of the age group 18-25, of our teaching institution, in the study period and included 132 individuals into our study fitting with study criteria.
From the total number of 132 subjects, 89 (67.4%) were male and 43 (32.6%) were female. Among all the subjects 92 subjects (67.4%) were normal, 30 (25%) had grade 1 fatty change, 10 (7.6%) had grade 2 fatty change. Furthermore,the frequency distribution of the hepatic sonographic findings among male & female subjects was done which is shown in tabular format (vide Table-1). Anthropometric details of the study population is given in a table-2(vide table-2)
Table1: Distribution of gender variable in case of normal findings, Grade 1 fatty change, Grade 2 fatty change
| Normal | Male | Female | Total |
| 63
(71%) |
29
(67.4%) |
92
(69.7%) |
|
| Grade 1 fatty grade | 19
(20%) |
11
(25.6%) |
30
(22.7%) |
| Grade 2 fatty grade | 7
(9%) |
3
(7 %) |
10
(7.6%) |
| Total | 89
(100%) |
43
(100%) |
132
(100%) |
Table 2: Distribution (Mean ± SD) of the following Anthropometric variables in case of normal findings,Grade 1 fatty change, Grade 2 fatty change.
| Anthropo-metric Variable |
Normal Mean ± S.D. |
Grade1fatty change Mean ± S.D. |
Grade 2 fatty change Mean ± S.D. |
| Height (cm) | 162.144±8.392 | 167.054±9.375 | 169.625±7.227 |
| Weight (kg) | 62.430±10.719 | 74.070±9.327 | 73.750±6.702 |
|
BMI (kg/ m2) |
23.616±2.865 | 26.357±2.530 | 25.628±0.940 |
Using Chi-Square (χ2) test for independence, it was found that there is no significant association between hepatic steatosis and sex distribution p-value-0.238).
For further ease of analysis, both grade -1 and grade-2 fatty change are combined under NAFLD. As subjects having grade 2 fatty liver is less innumber, we have merged both grade 1 and grade 2 fatty liver under the broad heading NAFLD group.
It is observed that in the NAFLD group AST: ALT is 0.9 which is less than 1. This finding is more in favor of a diagnosis of NAFLD than alcoholic liver disease and other advanced liver disease21. In alcoholic liver disease synthesis of a mitochondrial isoform of AST is increased which has longer half-life than the cytoplasmic isoform of AST. So, in alcoholic liver disease, AST to ALT ratio is usually greater than 114.
Cut off value of Insulin resistance in this study population is determined by ROC (Receiver Operating Characteristic) curve. The area under the curve is 0.937 which is nearer to 1. So, the accuracy of the test is very good.The cut-off value of IR in the present study population is determined to be 1.525 by matching the highest value of sensitivity with the lowest value of 1- sensitivity (p-value < 0.001). (Vide figure-1)
Using unpaired student’s t-test it has been found that there are significant differences between the mean values of ALT, AST, GGT, IR in normal subjects and subjects having NAFLD. Difference is significant at the (p < 0.001) level (Vide table-3).
Table 3: Comparison of the mean values of Liver enzymes (ALT, AST, GGT) & IR (HOMA-IR) between Normal and NAFLD group (unpaired Student’s t test)
|
Parameters |
Normal (92) Mean ±SD |
NAFLD (40) Mean ± SD |
t value |
P value |
| ALT (IU/ lt) | 28.599 ±15.491 | 51.450 ±18.134 | -7.389 | <0.001** |
| AST (IU/ lt) | 27.323 ±15.626 | 43.675 ±18.148 | -5.257 | <0.001** |
| GGT (IU/ lt) | 12.349 ± 4.878 | 23.168 ± 11.179 | -7.763 | <0.001** |
| IR (HOMA-IR) | 1.164 ± 0.548 | 2.057± 0.595 | -8.389 | <0.001** |
Another grouping was done using the cutoff value of Insulin Resistance (1.525) among study subjects and significant differences are found between the mean values of ALT, AST, and GGT among the two groups. (I.e. without Insulin Resistance and Those who have Insulin Resistance more than the Cut-Off). Difference is significant at the (p < 0.001) level (Vide table-4).
Table 4: Comparison of the mean values of Liver enzymes (ALT, AST, GGT) between groups (IR ≥ 1.525) & (IR<1.525) (unpaired Student’s t test).
| Parameters | IR ≥ 1.525 (42) Mean ±SD | IR<1.525 (90) Mean ± SD | t value | P value |
| ALT (IU/ lt) | 51.024 ±18.130 | 28.291 ±15.340 | 7.476 | <0.001** |
| AST(IU/ lt) | 43.905 ±18.319 | 26.852 ±15.152 | 5.627 | <0.001** |
| GGT(IU/ lt) | 22.725± 11.012 | 12.316±5.002 | 7.485 | <0.001** |
By both Kendall’s tau_b and Spearman’s rho correlation test, it is found that there is significant positive concordance between liver enzymes ALT, GGT, and hepatic steatosis in subjects having insulin resistance ≥ 1.525 (Vide table-5).
Table5: Showing correlation between Hepatic Steatosis& Liver enzymes (ALT, AST, GGT) in subjects having insulin resistance ≥ 1.525
|
Hepatic Steatosis |
Kendall’stau_b Correlation coefficient (r) |
ALT | AST | GGT |
|
0. 350**
|
0.140 | 0.426** | ||
|
Significance (p) 2- tailed |
0.007 | 0.281 | 0.001 | |
| Spearman’s rhoCorrelation coefficient (r) | 0.421** | 0.169 | 0.514** | |
| Significance
(p) 2- tailed |
0.005 | 0.286 | 0.001 |
Binary logistic regression analysis with stepwise adjustment added more strength to the findings of the correlation study. It was found that the odds of developing hepatic steatosis with One-unit higher ALT values in the total study population (n = 132) was 1.072 whereas for GGT it was 1.3, with the predictability 78.8 % vs 85.6 % for ALT to GGT. When the statistical model further narrowed that down to the population with Insulin Resistance (i.e. n = 42), the Odds for GGT increases significantly to 1.532 (p = 0.03) with the predictability of developing hepatic fatty changes 92.29% which is better than the same adjustment for ALT i.e. 90.2%. Hence it can be said that within our study population, in presence of insulin resistance, subjects having higher GGT values, rather ALT, can possess a greater risk of developing Steatotic changes, comparing the Odds (GGT to ALT 1.532 vs 1.067) (vide table-6).
Table 6: Showing Odds ratio for development of fatty changes in different statistical models using Binary Logistic regression.
| Parameters | Odds for Developing Hepatic Fatty changes | Significance
(P value) |
Nagelkerke R2 for Model Summary | Predictability Percentage |
|
ALT (n= 132) |
1.072 | < 0.001 | 0.376 |
78.8% |
|
GGT(n= 132) |
1.3 | < 0.001 | 0.469 |
85.6% |
| ALT in presence of IR
( > 1.525) (n= 42) |
1.067 | 0.19 | 0.525 | 90.2% |
| GGT in presence of IR
( > 1.525) (n= 42) |
1.532 | 0.03* | 0.572 | 92.29% |
Discussion
Prevalence of NAFLD is increasing in adolescents and the young population nowadays. Previous studies have been shown that NAFLD may advance to more severe hepatic conditions like cirrhosis, liver failure, and hepatocellular carcinoma. A strong association of NAFLD and metabolic syndrome has been found1-3so that often NAFLD is addressed as a hepatic presentation of metabolic syndrome.
NAFLD also represent as an important self-governing risk for the development of Cardiovascular disease (CVD). Several recent longitudinal studies have shown that CVD and atherosclerosis are important causes of morbidity and mortality in patients with NAFLD14. The liver is the center forthe production of classical biomarkers of inflammation and endothelial dysfunction. It has been shown that fibrinogen and CRP levels, which, known CVD risk factors, are increased in NAFLD patients, particularly in those with NASH 22.
Insulin resistance plays a major role in both NAFLD and metabolic syndrome. Both peripheral and hepatic insulin resistance is present in patients with NAFLD, irrespective of the coexistence of impaired glucose tolerance or obesity. Insulin resistance contributes to increased blood glucose level which in turn produces free fatty acids (FFA). Excess FFAs are not taken up by peripheral adipocytes and myocytes, instead of stored as diacyl and triacyl-glycerol in hepatocytes leading to the development of steatosis 23. Such Insulin resistance is regulated by both genetic and acquired factors which in turn influence the complications developed from insulin resistance19. It is associated with many serious medical conditions such as type 2 diabetes mellitus, cerebrovascular and coronary artery diseases, neurodegenerative disorders, etc. The association between insulin resistance and increased cardiovascular disease is mediated mainly at the genetic level. Insulin resistance leading to impaired nitric oxide-mediated vasorelaxation may contribute to hypertension and increased risk of atherosclerosis24.
The study population includes 132 medicos aged between 18 to 25 years. Details of the demographic distribution of the study population are discussed in the results and analysis section.
Though Ludwig in the definition of NAFLD stated that it is more common in women than in men25and in older studies also NAFLD was more frequent in women, the present study is not in agreement with this finding. In the present study, it has been seen that there is no significant association between hepatic steatosis and sex distribution.“TheDionysos study” also states that gender is not a risk factor for NAFLD in the general population1,4.
In the present study, it has been observed that healthy individuals had lower values of AST, ALT, GGT& IR than subjects having hepatic steatosis. [ (AST- 27.323 ± 15.626 vs 43.675 ± 18.148 IU/lt), (ALT- 28.599 ± 15.491 vs 51.450 ± 18.134 IU/lt), (GGT- 12.349 ± 4.878 vs 23.168 ± 11.179 IU/lt), (IR- 1.164± 0.548 vs 2.057 ± 0.595). The difference between the mean values of AST, ALT, GGT & IR among the two groups is significant at the level of P-value <0.01.
The further grouping was done using the cutoff value of Insulin Resistance (1.525) and a significant difference was found between the means values of ALT, AST, GGT among two groups (i.e. with Insulin Resistance ≥ 1.525 and those having Insulin Resistance < 1.525). [ (AST- 43.905 ± 18.319 vs 26.852 ± 115.152 IU/lt), (ALT- 51.024 ± 18.130vs 28.291± 15.340 IU/lt), (GGT- 22.725 ± 11.012 vs 12.316 ± 5.002 IU/lt)] The difference between the mean values of AST, ALT&GGT among two groups are significant at the level of P-value <0.01.
A good number of studies were conducted in western countries as well as in India which established that NAFLD is frequently associated with higher values of liver enzymes. R. Haring, H. Wallaschofski et al. in 2009 found in their study that GGT is frequently elevated in NAFLD and may also be a marker of increased mortality13. S. Akila, R. Deepti et al also concluded in their study in 2014 that NAFLD with MetS had increased serum GGT level 26. Both studies support the finding of the present study. Iqbal MurshedKabir et al also found in their study that the mean values of ALT and AST were much higher than the reference range in patients with NAFLD12. But the study of A. Wieckowska, A.E. Feldstein et al contradict the finding of the present study. In their study, more than two-thirds of NAFLD patients were found to have normal aminotransferase levels27. In another study, it was found that the entire histological spectrum of NAFLD can be observed in patients with normal ALT values28.In many previous studies, it was reported that MetS which is also known as Insulin Resistance syndrome is associated with abnormal liver function tests. AST, ALT, and GGT levels are high in patients of MetS, especially with high BMI15.Results from the cross-sectional study of S. Perera, V. Lohsoonthorn is also unison29.
Further statistical analysis has been done to find out is there any Enzyme better correlating with hepatic steatosis than others in the Scenario of Insulin Resistance and an interesting finding came into the light. Let’s explore that in further discussion.
When both Kendall’s tau_b and Spearman’s rho correlation test performed it was found that there is significant concordance (p value<0.01) between liver enzymes ALT and GGT and hepatic steatosis in subjects having insulin Resistance (>1.525) but not with AST (p-value = 0.286). The correlation coefficient (i.e. r) is found to be higher incase of GGT than ALT in both the test (vide Table-5).The finding implies that GGT has more positive concordance with NAFLD than ALT in the scenario of insulin resistance.
Having ALT and GGT positively correlating with hepatic steatosis in presence of insulin resistance, further Binary Logistic Regression with stepwise adjustment has been performed to ascertain which one of them predicts better about the development of fatty changes in this scenario. It has been observed that with Higher GGT values stronger predictability was found with hepatic steatosis than ALT among subjects having insulin resistance > 1.525 (p-value 0.03). A very few studies are found to directly or indirectly support the finding of the present study. R. Haring, H. Wallaschofski et al. in 2009 found in their study that GGT is frequently elevated in NAFLD and may also be a marker of increased mortality13. S. Akila, R. Deepti et al also concluded in their study in 2014 that NAFLD with MetS had increased serum GGT level26. Oxidative stress is pretty high in hepatic steatosis mediated by fat accumulation inside hepatocytes and been associated with hepatic insulin resistance. GGT is a cell-surface enzyme which primarily maintains intracellular defense against oxidative stress. So GGT is often found to be chronically elevated in NAFLD. Increased GGT level not only reflects the hepatic oxidative stress but also its association with insulin resistance. In studies of Koushik GG, Sharm S et al. (2009), it was concluded there is a significant positive correlation between GGT and Insulin resistance among all the liver enzymes, and monitoring GGT and fasting insulin levels might help to prevent the development of diabetes in obese children30. In a few previous studies elevated GGT level has been reported to be of prognostic significance of coronary artery disease which is an important complication of long-standing NAFLD. A positive correlation between elevated GGT level and Framingham cardiovascular risk scoring system has also been observed.Tara M. Wallace, Kristina M. Utzschneide et al also found in their study, that GGT was positively correlated with hepatic steatosis and associated with insulin sensitivity and glucose tolerance in both men and women. They also concluded that although GGT has been widely used as a specific biomarker of alcoholic liver disease, it has recently been found to be related to an increased risk of development of type 2diabetes, irrespective of alcohol intake as well as an increased risk of hypertension and cardiovascular mortality31.
Conclusion
Not only a good positive correlation found between Liver enzymes ALT and GGT with hepatic steatosis but also an interesting finding was established that subjects having higher GGT values rather than ALT possessa greater risk of developing steatohepatic changes in insulin-resistant background. Such observations add an extra edge to the pathophysiological understanding of NAFLD.
Although GGT has been widely used as a marker of severity of alcoholic liver disease, the present study observes that it has a potential to be used as a novel marker for assessing the severity of NAFLD in context with the insulin-resistant condition. On the other-hand, these observations also raise a question that can GGT be considered as the specific marker only for Alcoholic liver disease or it should be generalized as a marker for assessing the severity of fatty liver disease irrespective of the etiopathogenesis.
Considering the present study as a pilot one, further studies can be done on the general population to establish ranges and changes in GGT levels in fatty liver diseases of different etiologies and correlating them with previous observations. Moreover, studies can also be conducted in favor of GGT as a marker for monitoring the risks of cardiovascular, cerebrovascular, and severe hepatic complications in patients of NAFLD along with Insulin Resistance.
Acknowledgement
We take the opportunity to express our sincere gratitude to Dr. Asit Chandra Roy, Associate Professor, Department of Radio-diagnosis, North Bengal Medical College & Hospitalfor his advice and assistance in the radiological data. We also extend our extreme gratefulness to all the medicos who volunteered themselves for our study. This study would not have been possible without their kind co-operations.
Financial Support and Sponsorhip
There are no Financial support
Conflict of Interest
Authors declare there is no conflict of interest
References
- Paschos P, Paletas K. Nonalcoholic fatty liver disease and metabolic syndrome. Hippokratia. 2009;13(1):9.
- Bugianesi E, Leone N, Vanni E, Marchesini G, Brunello F, Carucci P, Musso A, De Paolis P, Capussotti L, Salizzoni M, Rizzetto M. Expanding the natural history of nonalcoholic steatohepatitis: from cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology. 2002;123(1):134-40.
CrossRef - Adams LA, Lymp JF, Sauver JS, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129(1):113-21.
CrossRef - Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology. 2005;42(1):44-52.
CrossRef - Singh SP, Singh A, Misra D, Misra B, Pati GK, Panigrahi MK, Kar SK, Bhuyan P, Pattnaik K, Meher C, Agrawal O. Risk factors associated with non-alcoholic fatty liver disease in Indians: a case–control study. Journal of clinical and experimental hepatology. 2015;5(4):295-302.
CrossRef - Singh SP, Nayak S, Swain M, Rout N, Mallik RN, Agrawal O, Meher C, Rao M. Prevalence of nonalcoholic fatty liver disease in coastal eastern India: a preliminary ultrasonographic survey. Tropical gastroenterology: official journal of the Digestive Diseases Foundation. 2004;25(2):76-9.
- Madan K, Batra Y, Gupta SD, Chander B, AnandRajan KD, Tewatia MS, Panda SK, Acharya SK. Non-alcoholic fatty liver disease may not be a severe disease at presentation among Asian Indians. World journal of gastroenterology. 2006;12(21):3400.
CrossRef - Day CP. james OF. Steatohepatitis: a tale of two “hits. 1998; 842-5.
CrossRef - Bajaj S, Nigam P, Luthra A, Pandey RM, Kondal D, Bhatt SP, Wasir JS, Misra A. A case-control study on insulin resistance, metabolic co-variates & prediction score in non-alcoholic fatty liver disease. Indian Journal of Medical Research. 2009;129(3):285.
- Sanyal AJ, Campbell–Sargent C, Mirshahi F, Rizzo WB, Contos MJ, Sterling RK, Luketic VA, Shiffman ML, Clore JN. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120(5):1183-92
CrossRef - Patell R, Dosi R, Joshi H, Sheth S, Shah P, Jasdanwala S. Non-alcoholic fatty liver disease (NAFLD) in obesity. Journal of clinical and diagnostic research: JCDR. 2014;8(1):62.
CrossRef - Kabir IM, Alam M, Mahmuduzzaman M, Al Mamoon A, Ahmed MU, Safwath SA. Correlation between bright echogenic liver, elevated liver enzymes and liver histology. Journal of Dhaka National Medical College & Hospital. 2011;17(1):8-13.
CrossRef - Haring R, Wallaschofski H, Nauck M, Dörr M, Baumeister SE, Völzke H. Ultrasonographic hepatic steatosis increases prediction of mortality risk from elevated serum gamma‐glutamyltranspeptidase levels. Hepatology. 2009;50(5):1403-11.
CrossRef - Ghouri N, Preiss D, Sattar N. Liver enzymes, nonalcoholic fatty liver disease, and incident cardiovascular disease: a narrative review and clinical perspective of prospective data. Hepatology. 2010;52(3):1156-61.
CrossRef - Hsieh MH, Ho CK, Hou NJ, Hsieh MY, Lin WY, Yang JF, Chiu CC, Huang JF, Chang NC, Wang CL, Dai CY. Abnormal liver function test results are related to metabolic syndrome and BMI in Taiwanese adults without chronic hepatitis B or C. International journal of obesity. 2009;33(11):1309.
CrossRef - Burtis CA, Ashwood ER, Bruns DE. Tietz textbook of clinical chemistry and molecular diagnostics-e-book. Elsevier Health Sciences; 2012.
- Kaushik GG, Sharm S, Sharma R, Mittal P. Association between gamma glutamyl transferase and insulin resistance markers in healthy obese children. J Assoc Physicians India. 2009;57;695-8.
- Campos SP, Baumann H. Insulin is a prominent modulator of the cytokine-stimulated expression of acute-phase plasma protein genes. Molecular and cellular biology. 1992;12(4):1789-97.
CrossRef - Sivapackianathan R, Asivatham AJ, Al-Mahtab M, Chowdhury TA. Association between non-alcoholic fatty liver disease and metabolic syndrome. International Journal of Hepatology. 2010;1(4):17-24.
- Bae JC, Suh S, Park SE, Rhee EJ, Park CY, Oh KW, Park SW, Kim SW, Hur KY, Kim JH, Lee MS. Regular exercise is associated with a reduction in the risk of NAFLD and decreased liver enzymes in individuals with NAFLD independent of obesity in Korean adults. PloS one. 2012;7(10)e46819.
CrossRef - Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999;30(6):1356-62.
CrossRef - Yoneda M, Mawatari H, Fujita K, Iida H, Yonemitsu K, Kato S, Takahashi H, Kirikoshi H, Inamori M, Nozaki Y, Abe Y. High-sensitivity C-reactive protein is an independent clinical feature of nonalcoholic steatohepatitis (NASH) and also of the severity of fibrosis in NASH. Journal of gastroenterology. 2007;42(7):573-82.
CrossRef - Day C. Non-alcoholic steatohepatitis (NASH): where are we now and where are we going?Gut 2002; 50: 585-88.
CrossRef - Abel ED, O’Shea KM, Ramasamy R. Insulin resistance: metabolic mechanisms and consequences in the heart. Arteriosclerosis, thrombosis, and vascular biology. 2012;32(9):2068-76.
CrossRef - Ludwig J, Viggiano TR, Mcgill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clinic Proceedings 1980; (Vol. 55, No. 7, pp. 434-438).
- Akila S, Deepti R, Ramesh L, Saritha B. The impact of increased serum GGT levels and NAFLD on the components of Metabolic Syndrome. Journal of current trends in clinical medicine & laboratory Biochemistry. 2014;2(4):34-38.
- Wieckowska A, Feldstein AE. Diagnosis of nonalcoholic fatty liver disease: invasive versus noninvasive. InSeminars in liver disease 2008; (Vol. 28, No. 04, pp. 386-395).
CrossRef - Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA, Sterling RK, Shiffman ML, Stravitz RT, Sanyal AJ. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37(6):1286-92.
CrossRef - Perera S, Lohsoonthorn V, Jiamjarasrangsi W, Lertmaharit S, Williams MA. Association between elevated liver enzymes and metabolic syndrome among Thai adults. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2008;2(3):171-8.
CrossRef - Kaushik GG, Sharm S, Sharma R, Mittal P. Association between gamma glutamyl transferase and insulin resistance markers in healthy obese children. J Assoc Physicians India. 2009;57;695-8.
- Wallace TM, Utzschneider KM, Tong J, Carr DB, Zraika S, Bankson DD, Knopp RH, Kahn SE. Relationship of liver enzymes to insulin sensitivity and intra-abdominal fat. Diabetes care. 2007;30(10):2673-8.
CrossRef

This work is licensed under a Creative Commons Attribution 4.0 International License.





