How to Cite | Publication History | PlumX Article Matrix
Kanak Mahajan1 , Meenakshi Bhagat2
, Meenakshi Bhagat2 , Jessica Cherukuri1
, Jessica Cherukuri1 , Rahul Gupta3, Amrit Sudershan1,4
, Rahul Gupta3, Amrit Sudershan1,4 , Rakesh Kumar Panjaliya1
, Rakesh Kumar Panjaliya1 and Parvinder Kumar1,2
and Parvinder Kumar1,2
1Institute of Human Genetics, University of Jammu, J and K, India.
2Department of Zoology, University of Jammu, J and K, India.
3Department of Urology, Govt. Super Specialty Hospital, Jammu, India.
4Department of Human Genetics, Sri Pratap College, Cluster University of Srinagar, Kashmir, J and K, India
Corresponding Author E-mail: parvinderkb2003@gmail.com
DOI : http://dx.doi.org/10.13005/bbra/3140
ABSTRACT: The current study sought to identify and quantify the prevalence of various risk factors for nephrolithiasis in the population of Jammu region. In the present study, a total of 100 study participants (50 cases and 50 controls) were enrolled. A detailed health questionnaire covering different risk factors viz., socio-demographic, biochemical, clinical and lifestyle parameters were designed for the study. The results revealed a significant association between physical inactivity and risk of nephrolithiasis. On comparison of biochemical parameters between the male and female patients, it was observed that overall male patients have slightly higher mean values of biochemical factors. Water being an important factor for reducing the risk of kidney stone but the consumption of water is also low (less than 3 liters/day) in most of the patients.
KEYWORDS: Cases; Controls; Nephrolithiasis; Socio-Demographic Parameters; Statistical Analysis
Download this article as:| Copy the following to cite this article: Mahajan K, Bhagat M, Cherukuri J, Gupta R, Sudershan A, Panjaliya R. K, Kumar P. Identification and Assessment of Non-Genetic Factors Contributing to Nephrolithiasis (Kidney Stone) in the Jammu Region. Biosci Biotech Res Asia 2023;20(3). |
| Copy the following to cite this URL: Mahajan K, Bhagat M, Cherukuri J, Gupta R, Sudershan A, Panjaliya R. K, Kumar P. Identification and Assessment of Non-Genetic Factors Contributing to Nephrolithiasis (Kidney Stone) in the Jammu Region. Biosci Biotech Res Asia 2023;20(3). Available from: https://bit.ly/3LmggsH |
Introduction
Nephrolithiasis commonly known as kidney stone is a global problem affecting people of various age groups, gender and ethnicity. There has been a global increase in its occurrence in the previous several decades 1,2 and epidemiological studies have suggested that the prevalence is higher in the Indian population which is estimated to be 7.9% 3. Among Indian population, the incidence rates are higher in North Indian regions 4.
Crystals in the kidneys as a result of dissolved minerals in the urine can be caused due to the environmental, metabolic as well as genetic factors 5. Also, it has become one of the most frequent diseases that pose a severe threat to human health, as a result of rising economic status and changes in people’s lifestyles and food arrangements 6. There is ample evidence that suggests that systemic illnesses such as diabetes mellitus (Type II), dyslipidemia, obesity, and hypertension can all cause nephrolithiasis 7.
It has also been observed that people of all ages are affected, but those between the ages of 30 and 60 are the most affected age groups 8. The disease burden of kidney stone disease in men and women varies throughout time. In comparison to previous generations, the latter, particularly adolescent females, are more prone to acquire kidney stone disease during the course of their lives 9.
As presence of kidney stones is prevalent condition that can lead to serious complications, the goal of this study was to determine the risk factors their relationship with nephrolithiasis among patients from the Jammu region UT J & K.
Materials and Methods
The study was initiated after obtaining the ethical clearance from the Institutional Ethical Committee University of Jammu (RA/19/3/20) as well as from Government Medical College, Jammu (JMC/UG/506). The study consisted of 100 participants (50 cases and 50 healthy, unrelated controls). Inclusion and exclusion criteria were also set during the process. Inclusion criteria: 1. All the cases that were confirmed via radiographic assessment and ultrasonography were only considered as patients. 2. The patients above the age of 18 years were considered. 3. Both male and female subjects.
Exclusion criteria: 1. Patients with severe renal failure. 2. Patients with chronic urinary system disorders or other chronic illness 3. Pregnant women. 4. Patients belonging to any region except Jammu were also excluded.
Data Collection
A detailed pre-designed health questionnaire, including parameters such as socio-demographic factors, lifestyle risk factors comorbid conditions like hypertension and diabetes, other factors including source of drinking water, water intake, different clinical parameters (urination and site of kidney stones) was duly filled from each individual.
Biochemical profiling
The urine analysis and biochemical profiling of patients was done by the Super specialty hospital.
Statistical Analysis
For non- genetic variables, mean and Standard deviation were calculated and paired t-test was performed to calculate the difference between the patients and controls. To calculate mean and standard deviation freely available online software such as GraphPads QuickCalcs software (https://www.graphpad.com/quickcalcs/ttest2/) was used. To assess the association of Nephrolithiasis risk, odds ratios (OR) with 95% CI were calculated by using online software MedCalc software (http://www.medcalc.org/calc/odds_ratio.php). A p-value of <0.05 was considered as statistically significant.
Results
Socio-demographic profiling
In the present study, we enrolled 50 kidney stone patients (28 males & 22 females) and 50 healthy unrelated controls (21 males & 29 females). The mean age of onset of Nephrolithiasis was 39.32±13.22 years for males and 37.91±14.09 years for females. On observing educational profile of the study participants, it was observed that individuals with higher qualification were present in controls 60% and in patients it was 26%. In case of middle level qualification, the patients (40%) were more than controls (12%). In primary level of education controls (20%) were more as compared to patients (10%). Majority of our studied subjects were married (Patients=74% and controls=60%). Consanguinity practice was present with a rate of 14.28% in male patients and in controls consanguinity rate was 11.76% in males. Consanguinity was completely absent in females both in patients as well as controls. Maximum disease load was observed in patients residing in rural areas of Jammu region i.e., 74% and 26% from urban counterparts of Jammu region. The Socio- demographic parameters of the enrolled individuals were summarised in Table 1.
Table 1: Socio- demographic parameters of study participants.
| Parameter | Patients | Controls | |||||
| Men (n=28)
|
Women (n=22) | Total (N=50) | Men (n=21) | Women (n=29) | Total (N=50) | ||
| Age | Mean | 39.32±13.22 | 37.91±14.09 | 38.32±13.77 | 37.10±7.22 | 30.24±10.07 | 33.98±10.23 |
| Dwelling | Urban | 5(17.86%) | 8(36.36%) | 13(26%) | 8(38.09%) | 15(51.72%) | 23(46%) |
| Rural | 23(82.14%) | 14(63.64%) | 37(74%) | 13(61.91%) | 14(48.28%) | 27(54%) | |
| Marital
status |
Single | 7(25%) | 6(27.27%) | 13(26%) | 4(19.05%) | 16(55.17%) | 20(40%) |
| Married | 21(75%) | 16(72.73%) | 37(74%) | 17(80.95%) | 13(44.83%) | 30(60%) | |
| Consanguinity | Yes | 3(14.29%) | 0 | 3(8.10%) | 2(11.76%) | 0 | 2(40%) |
| No | 18(85.71%) | 16(100%) | 34(91.90%) | 15(88.24%) | 13(100%) | 30(60%) | |
| Educational
status |
Higher | 3 (10.72%) | 10(45.45%) | 13(26%) | 10(47.62%) | 20(68.97%) | 30(60%) |
| Middle | 17(60.71%) | 3(13.64%) | 20(40%) | 4(19.05%) | 2(6.90%) | 6(12%) | |
| Primary | 1(3.57%) | 4(18.18%) | 5(10%) | 6(28.57%) | 4(13.79%) | 10(20%) | |
| Uneducated | 7(25%) | 5(22.73%) | 12(24%) | 1(4.76%) | 3(10.34%) | 4(8%) | |
Lifestyle risk factors
A variety of lifestyle or behavioural characteristics that can have a substantial impact on a person’s health were explored in the current study and are enlisted in Table 2. OR analysis was also carried out to explore the association of these risk factors with the development of kidney stones (Table 3). The prevalence of smoking was higher in controls (12%) than in patients (10%). The prevalence of tobacco chewing in patients was 6%. Among our study subjects, the incidence of alcohol intake was higher in controls (16%) than in Nephrolithiasis patients (8%). Women participants of our study were not reported to be engrossed in smoking, chewing tobacco and drinking habit due to cultural perspective. The OR analysis depicted that smoking, chewing tobacco and alcohol intake were not adding a significant risk to the development of kidney stone.
Table 2: Prevalence of Lifestyle risk factors in study participants.
| Parameter | Patients | Controls | |||||
| Men
(n=28) |
Women
(n=22) |
Total
(N=50)
|
Men
(n=21) |
Women
(n=29) |
Total
(N=50) |
||
| Diet | Non
Vegetarian |
19(67.86%) | 10(45.45%) | 29(58%) | 14(66.67%) | 14(48.28%) | 28(56%) |
| Vegetarian | 9(32.14%) | 12(54.55%) | 21(42%) | 7(33.33%) | 15(51.72%) | 22(44%) | |
| Junk food | Never | 10(35.71%) | 11(50%) | 21(42%) | 11(52.38%) | 13(44.83%) | 24(48%) |
| Rarely | 15(53.57%) | 11(50%) | 26(52%) | 7(33.33%) | 13(44.83%) | 20(40%) | |
| Usually | 3(10.72%) | 0 | 3(6%) | 3(14.29%) | 3(10.34%) | 6(12%) | |
| Salt
consumption |
Low | 5(17.86%) | 5(22.72%) | 10(20%) | 4(19.05%) | 6(20.69%) | 10(20%) |
| Average | 20(71.43%) | 14(63.64%) | 34(68%) | 14(66.66%) | 20(68.97%) | 34(68%) | |
| High | 3(10.71%) | 3(13.64%) | 6(12%) | 3(14.29%) | 3(10.34%) | 6(12%) | |
| Smokers | Yes | 5(17.86%) | 0 | 5(10%) | 6(28.57%) | 0 | 6(12%) |
| No | 23(82.14%) | 22(100%) | 45(90%) | 15(71.43%) | 29(100%) | 44(88%) | |
| Alcohol | Yes | 4(14.29%) | 0 | 4(8%) | 8(38.10%) | 0 | 8(16%) |
| No | 24(85.71%) | 22(100%) | 46(92%) | 13(61.90%) | 29(100%) | 42(84%) | |
| Tabacco | Yes | 3(10.71%) | 0 | 3(6%) | 0 | 0 | 0 |
| No | 25(89.29%) | 22(100%) | 47(94%) | 21(100%) | 29(100%) | 50(100%) | |
| Physical
activity |
Yes | 7(25%) | 10(45.45%) | 17(34%) | 15(71.43%) | 13(44.83%) | 28(56%) |
| No | 21(75%) | 12(54.55%) | 33(66%) | 6(28.57%) | 16(55.1%) | 22(44%) | |
| Caffeine intake
(Tea per day) |
Low consumers
(0-2cups) |
6(21.43%) | 7(31.82%) | 13(26%) | 3(14.29%) | 5(17.24%) | 8(16%) |
| High consumers
(more than 2cups) |
22(78.57%) | 15(68.18%) | 37(74%) | 18(85.71%) | 24(82.76%) | 42(84%) | |
|
Comorbidity |
Hypertension
Yes
|
6(21.42%) | 2(9.09%) | 8(16%) | 0 | 0 | 0 |
| No | 22(78.57%) | 20(90.90%) | 42(84%) | 21(100%) | 29(100%) | 50(100%) | |
| Diabetes Yes |
1(3.58%) | 1(4.55%) | 2(4%) | 0 | 0 | 0 | |
| No | 27(96.42%) | 21(95.45%) | 48(96%) | 21(100%) | 29(100%) | 50(100%) | |
Table 3: Association of different risk factors with Nephrolithiasis.
| Parameters | Patients
(N=50) |
Controls
(N=50) |
Odds ratio
(95% CI) |
P-value | |
| Smoking | Yes | 5(10%) | 6(12%) | 0.81(0.23-2.86) | 0.74 |
| No | 45(90%) | 44(88%) | Ref. | ||
| Tobacco | Yes | 3(6%) | 0 | 7.44(0.37-147.93) | 0.18 |
| No | 47(94%) | 50(100%) | Ref. | ||
| Alcohol | Yes | 4(8%) | 8(16%) | 0.45(0.12-1.62) | 0.22 |
| No | 46(92%) | 42(84%) | Ref. | ||
| Physical
activity |
Yes | 17(34%) | 28(56%) | Ref. | |
| No | 33(66%) | 22(44%) | 2.47 (1.10-5.55) | 0.03* | |
|
Diet |
Non
vegetarian |
29(58%) | 28(56%) | 1.13(0.51-2.52) | 0.74 |
| Vegetarian | 21(42%) | 22(44%) | Ref. | ||
|
Junk food |
Never | 21(42%) | 24(48%) | Ref. | |
| Rarely | 26(52%) | 20(40%) | 1.48(0.65-3.39) | 0.34 | |
| Usually | 3(6%) | 6(12%) | 0.57(0.12-2.57) | 0.46 | |
| Salt
consumption |
Low | 10(20%) | 10(20%) | 1 | – |
| Average | 34(68%) | 34(68%) | Ref. | ||
| High | 6(12%) | 6(12%) | 1 | – | |
| Caffeine intake (Tea- cups per day) | Low
consumers |
13(26%) | 8(16%) | Ref. | |
| High
consumers |
37(74%) | 42(84%) | 1.84(0.68-4.94) | 0.22 | |
*Significant P-value
The parameter of physical inactivity was found to be a prevalent risk factor associated with Nephrolithiasis in our study [OR=2.47, 95% CI (1.10- 5.55), p<0.03]. The prevalence of sedentary behaviour was higher in Nephrolithiasis patients (66%) in judgment to healthy controls (44%). Only 34% of Nephrolithiasis patients were engaged in exercise/walk/yoga which was lower than proportion of 56% of physically active controls. Mode of diet whether vegetarian or non- vegetarian is underlined in diet pattern in the present study. Ingestion of non-vegetarian diet was found to be higher in the patient group (58%) as compared to control group (56%). OR analysis showed that non-vegetarian diet was not significantly associated with the risk of kidney stone formation.
In the study subjects the intake of junk food was categorised under three categories individuals taking it rarely, usually and those who never consume junk food stuffs. The percentage of junk food consumers among study participants was as follows: rare consumers were 52% in patients and 40% in controls, usual consumers were 6% in patients and 12% in controls where as non-consumers were 42% in patients and 48% in controls. We did not find any association of junk food with susceptibility of kidney stone formation [rare consumers, OR=1.48(0.65- 3.39), p=0.34 and usual consumers, OR= 0.57(0.12-2.57), p=0.46]. Caffeine intake was recorded for study participants in terms of number of tea cups consumed per day. Caffeine intake incidence was found to be higher Nephrolithiasis patients (26%) in comparison to controls (16%) with OR more than 1 i.e. OR=1.84 (0.68-4.94) but it could not reach statistical significant value (p=0.22).
Biochemical Profiling
The biochemical profiling parameters of the enrolled patients (Table 4) shows that the mean haemoglobin (Hb) levels for both male patient and female patients were almost similar (males: 10.77±1.61 vs. females: 10.65±1.76; p=0.79). In the present study mean serum creatinine levels in men was 1.32±0.81 whereas in females it was 1.09±0.71 which was slightly lower than the males suffering from nephrolithiasis. High-sodium diet can trigger nephrolithiasis as it increases the amount of calcium in urine. In present work male patients (138.68±4.65 mg/L) had comparatively higher levels of sodium than female patients (136.82±3.95 mg/L). Potassium levels were also checked in the study participants and it was seen that study patients have higher levels of potassium out of which female (3.89±0.50) have slightly higher levels of potassium in comparison to males (3.77±0.46).
Table 4: Biochemical profiling of blood and urine.
| Parameters | Males | Females | Total | P value |
| Hemoglobin levels
(dL) |
10.77±1.61 | 10.65±1.76 | 10.80±1.69 | 0.79 |
| Creatinine | 1.32±0.81 | 1.09±0.71 | 1.21±0.73 | 0.36 |
| Sodium levels
(mg/L) |
138.68±4.65 | 136.82±3.95 | 137.85±4.29 | 0.18 |
| Potassium level
(L/d) |
3.77±0.46 | 3.89±0.50 | 3.82±0.47 | 0.29 |
Other parameters
Source of drinking water also aids in promoting Kidney stone formation. Different sources of drinking Water among enrolled patients are depicted in Figure 1. Majority of the patients consume tap water i.e., 51.85% for males and 30.43% for females. Following tap water, the second most common source of drinking water was hand pump which was consumed more by our female patients (34.78%) in comparison to male patients (14.81%). There was water intake from natural springs, 18% (male 18.51% & female 17.39%) as well as from wells 6% (male 18.51% &female 4.34%). There were 8% of the patients who were consuming filtered water (7.4% males & 8.69% females) and 2% consumed water from the pond (4.34% females and no males).
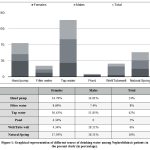 |
Figure 1: Graphical representation of different source of drinking water among Nephrolithiasis patients in the present study (in percentage). |
Daily water intake capacity of study patients was also recorded in the present study (Figure 2). It was observed that majority of the patients were taking water less than 3 litres/day (i.e., 74%) followed by 18% of patients taking water between 3-5 litres/day and only fewer no. of them i.e., 8% patients were consuming more than 5 litres of water per day. Male to female water intake percentage showed that 90.90% of females were drinking less than 3 litres of water per day in comparison to 60.71% of males. The patients whose water intake capacity was 3-5 litres/day and more than 5 litres/Day were more in males (28.57% & 4.55% respectively) than in females (10.72% & 4.55% respectively).
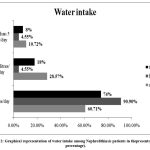 |
Figure 2: Graphical representation of water intake among Nephrolithiasis patients in thepresentstudy (in percentage). |
Comorbidities
The prevalence of diabetes mellitus as a risk factor for Nephrolithiasis was estimated in present patient subjects and it was found that only 4% of patients were diabetic whereas 96% of patients were non-diabetic. Among diabetic patients, 4.55% were females and 3.58% were males. Hypertension is often linked with Nephrolithiasis. In the present study it was revealed that majority of patient subjects were normotensive (males: 85.72%, females: 81.82%, total: 84%) and rest 16% of total patients were hypertensives (males: 14.28% and females: 18.18%)
Clinical parameters
The pattern of urination in enrolled patients was presented in Figure 3. It was observed that the urination was maximum (more than 5 times/day) in males (28.57%) than in females (27.27%). There were more female (45.46%) patients whose urination pattern was between (3-4 times/day) than males (42.86%). Among the least urination interval i.e., less than 3 times/day women (27.27%) were less in comparison with men (28.57%). Nephrolithiasis patient’s skin is pallor in comparison to healthy individuals. In the present study (Figure 4). Paleness was observed in 8% of total patients whereas 92% of patients were having normal skin colour. Pallor was found to be common in case of both, females (9.10%) as well as males (7.14 %).
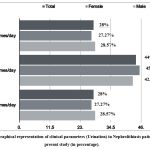 |
Figure 3: Graphical representation of clinical parameters (Urination) in Nephrolithiasis patients in the present study (in percentage). |
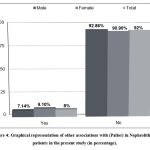 |
Figure 4: Graphical representation of other associations with (Pallor) in Nephrolithiasis patients in the present study (in percentage). Click here to view figure |
The occurrence of nephrolithiasis in individual acts as a risk factor which aids to its recurrence as well. In the present study, a large proportion of patients were first time stone formers (58.70%) in comparison to recurrent stone formers (41.30%). Frequency of recurrent stone formation was higher in males than in females (46.15% vs. 35% respectively) whereas as per first time stone formation was concerned it was observed that percentage was higher in female patients (65%) in contrast to male patients (53.85%) (Figure 5).
The position of stone can be checked by performing Imaging analysis. The positions which were analysed in present study were bilateral, right kidney, left kidney (Figure 6). Among the patients the majority of cases were having stone in right kidney (40.82%) mostly in females (42.86%) than males (39.29%). Following were left kidney (36.74%) stone patients in which males (39.29%) were more prone than females (33.33%). There were fewer patients who were suffering from bilateral (22.44%) kidney stone; more in female (23.81%) than male (21.42%).
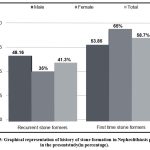 |
Figure 5: Graphical representation of history of stone formation in Nephrolithiasis patients in the presentstudy(in percentage). |
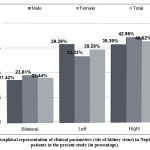 |
Figure 6: Graphical representation of clinical parameters (site of kidney stone) in Nephrolithiasis patients in the present study (in percentage). |
Discussion
Nephrolithiasis is a complex disease affected by several factors. There is paucity of the data regarding its prevalence and association of risk factors from the North Indian population of Jammu region. Taking this into consideration the present study was designed to identify the prevalence and association of different socio-demographic, biochemical and lifestyle parameters with Nephrolithiasis.
The Socio-demographic parameters that were promoting nephrolithiasis were sex, age, marital status, consanguinity, literacy rate, residential areas. Being educated helps people to understand about different aspects of disease. Health literacy among common people helps in disease prevention and health promotion. In the present investigation we observed that the majority of our study participants both patients and controls were educated and had better understanding of the disease.
Consanguinity increases the risk of inheriting diseases including nephrolithiasis. The risk is higher in case of 1st degree consanguinity. Studies have shown a genetic link between marriage and consanguinity for development of renal stones. In the present study the rate of consanguinity is higher in case of patients similar to the studies conducted by Yilmaz and Dorterler (2020), Maara et al., (2018) and Safadar et al., (2020) 10-12.
There are several epidemiological studies that demonstrates that the development of kidney stone is higher in case of males as compared to females as shown in our study 5,13. Furthermore, we noticed that the majority of enrolled patients were residents of rural parts of Jammu region. This can be because of the climate and the water supply of the areas as suggested by various studies by Alaya et al. (2011), Bajrami et al. (2012) and Hallawee (2015) 14-16.
Unhealthy lifestyle practices such as smoking, chewing tobacco, alcoholism, lack of physical activity, inadequate water intake and consumption of junk food are key contributors in the development of Nephrolithiasis. In the present study, prevalence of different lifestyle factors was evaluated to assess their association with the disease. The prevalence of smoking in our study was 10% and we did not find a significant association of smoking with Nephrolithiasis. Similarly, Moudi et al., (2017) reported lack of association of smoking with nephrolithiasis 13. Habit of chewing tobacco was also found not be associated with the risk of kidney stone formation in our study. Likewise, a study reported lower prevalence of tobacco consumption and the authors also declared that chewing tobacco was not associated with the risk of disease 17. In the case of alcohol consumption there has been no significant association with kidney stone in the present study and as reported by Zhao et al. (2015) 18.
Physical activity levels directly affect the body’s physiological waste excretion processes as well as the severity of metabolic illnesses like obesity and diabetes. While increasing the frequency of urine output, physical activity promotes people to drink more water. Nephrolithiasis risk would presumably be decreased by both of these conditions. As per dietary pattern was concerned, we observed that the percentage of junk food consumers (usual) was quite low in patients but consumption of non-vegetarian diet was higher in patients and this consumption of animal protein can have an acid loading effect on metabolism that can lead to the formation of stones in kidney 19-21.
Caffeine acts as a diuretic and it is known that the consumption of caffeine containing beverages like coffee, tea and cola to more than two cups per day causes the body to lose fluids too quickly and the urine to become too concentrated. Furthermore, both coffee and tea contain high levels of oxalate, a common component of kidney stones 5. In the present work the prevalence of caffeine intake was found to be higher in patients in comparison to controls.
Different biochemical parameters such as haemoglobin, sodium and potassium were considered in this investigation. A recent study found slightly higher serum creatinine levels in females compared to males. Our study reported lower levels of serum creatinine compared to the work conducted by Wozniak et al. (2018) 22. Additionally, males had slightly higher creatinine levels than female patients in our study. There was no significant difference in mean sodium levels between males and female patients in our study which is consistent with the findings of Hadian et al. (2018) 23. In terms of potassium levels, our study found high levels in urine in contradiction to the study by Grampsas et al. (2000) 24.
Other factors that were promoting the onset of Nephrolithiasis were source of drinking water, and quantity of water intake. In present study, source of drinking water was recorded in patients and it was found that among different types of sources, majority of the patients consume tap water, followed by hand pump water, then followed by natural springs, filtered water, wells and from pond. Prakash et al., (2019) also reported higher percentage of tap water and bore-well/ hand pump water as a source of drinking water in patients 25. There was no evidence of risk of stone formation found in relation to drinking tap water but it was reported in literature that consuming hard water promotes kidney stone formation 26 and soft water consumption can be advised to the stone formers to help stop the development of new stones 27.
To avoid the recurrence of kidney stone the American College of Physicians (ACP) and the American Urological Association (AUA) advised patients to drink enough water 28. This is because the volume of urine significantly affects the saturation of lithogenic salts such as calcium and uric acid 29-31. In the present study we observed that majority of the patients were taking water less than 3 litres/day which showed water intake adds to risk of Nephrolithiasis. Also, in an extensive cross-sectional analysis based on the NHANES 2009-2012 cycles, it was observed that improved hydration status and higher urine output was significantly linked with lower risk of nephrolithiasis 32.
Other complications associated with Nephrolithiasis were diabetes, hypertension, paleness of skin, history of stone formation (recurrent or first time stone former). There are several studies that show the independent association of hypertension and diabetes mellitus with nephrolithiasis 33-37. One potential connection between the two conditions can be the change in the chemical composition of urine 38. Similarly, diabetes mellitus is a condition that can lead to nephropathy, infections, and motility issues with the urinary system. Among the pathophysiological reasons underlying the development of stones in diabetes and hypertension are increased urine acidity, hypocitraturia, hyperoxaluria, hyperphosphaturia, and hypercalciuria 39. But, in the present study we recorded lower prevalence of comorbid conditions such as diabetes mellitus and hypertension with nephrolithiasis similar to the studies conducted by Sancak et al (2015) and Shoag et al. (2015) 38,40.
The clinical parameters associated with Nephrolithiasis were site of kidney stone (bilateral, right or left kidney) and pallor. Determination of stone location from imaging enables risk stratification regarding spontaneous stone passage without surgical intervention 41. The frequency of patients with right side kidney stone is higher followed by left side and then bilateral kidney stone in the current study. The results are lined up with the study done earlier by Ulusan et al. (2007) 42. Various studies suggested that one of the major problems with nephrolithiasis was the higher rate of recurrence but in the present study the recurrence rate of stone in patients is low. This result is in contradiction to the studies that revel the recurrence rate to be 50% in 5-10 years 43 and 75% over 20 years 25.
Conclusion
The overall consensuses of present work in Nephrolithiasis proves that there is no single contributing factor responsible for the development of Nephrolithiasis, but rather it is a combination of risk factors that can cause this disease. The present study is in fact a preliminary study which aimed to assess the prevalence of different non-genetic factors which are associated with kidney stones, as there is paucity of data on this topic from Jammu region. It was observed that the disease was prevalent in male as we reported higher no. of male patients during study period and also majority of the enrolled patients were residents of rural areas. Among lifestyle parameters, higher prevalence and a significant risk was observed for physical inactivity, caffeine intake and non-vegetarian diet towards kidney stone. Our findings did not support the notion that hypertension and diabetes increases the risk of kidney stones as we found lower frequency of these co-morbid conditions in present investigation. The present study also reported higher no. of patients with first time stone episodes and from the biochemical profiling, potassium levels were found to be higher.
In conclusion, the present study declares nephrolithiasis as a complex multifactorial heterogeneous disease whose etiology is influenced by variety of factors.
Limitations
The limitations in this study that should be considered are the sample size was limited as it is a preliminary study and the biochemical profiling was only available for patients not for controls, as a result of which we were not able to draw a definite relationship of this parameter with the risk of nephrolithiasis.
Future implications
The present study is an effort to generate the preliminary data on risk factors associated with the development of Nephrolithiasis (kidney stones) in Jammu region. This research work will be extended on larger study sample and also genetic factors (candidate genes) associated with this disease will be included.
Acknowledgement
The researchers are grateful to the study subjects for giving their data and medical history. The authors are grateful to the Coordinator, Institute of Human Genetics, the University of Jammu, for providing necessary facilities. Kanak Mahajan, also acknowledges the financial support from CSIR-UGC NET-JRF Fellowship.
Conflict of Interest
Kanak Mahajan carried out the extensive fieldwork and data compilation. Meenakshi Bhagat and Jessica Cherukuri were involved in compilation of the manuscript. Amrit Sudershan helped in the compilation of tables and images. Rahul Gupta, Parvinder Kumar and Rakesh Kumar Panjaliya have framed the work plan, provide guidance at every step and reviewed the article.
Funding Source
JK State Science and Innovation Council, Department of Science and Technology, Jammu & Kashmir (Order no. 80 of 2021).
References
- Taguchi K, Yasui T, Milliner DS, Hoppe B, Chi T. Genetic risk factors for idiopathic urolithiasis: a systematic review of the literature and causal network analysis. European urology focus. 2017; 3(1):72-81.
CrossRef - Thongprayoon C, Krambeck AE, Rule AD. Determining the true burden of kidney stone disease. Nature Reviews Nephrology. 2020; 16(12):736-46.
CrossRef - Faridi MS, Singh KS. Preliminary study of prevalence of urolithiasis in North-Eastern city of India. Journal of Family Medicine and Primary Care. 2020; 9(12):5939.
CrossRef - Talati JJ, Haroon N, Trinchieri A. Renal stone disease in different racial groups. Urolithiasis: basic science and clinical practice. 2012:107-10.
CrossRef - Sofia NH, Walter TM, Sanatorium T. Prevalence and risk factors of kidney stone. Global Journal for Research Analysis. 2016; 5(3):183-7.
- Kunjumon MK, Nayak SG, D’Souza JP. Knowledge on Urolithiasis among Patients Attending OPDs in Selected Hospital of Udupi District Karnataka. Indian Journal of Public Health Research & Development. 2020; 11(4).
- Abbas W, Akram M, Sharif A. Nephrolithiasis; prevalence, risk factors and therapeutic strategies: a review. Madridge J. Intern. Emerg. Med. 2019; 3:90-5.
CrossRef - Begum, K., Abbas Z., Umasri, N., and Mounika, K. Nephrolithiasis: An Update on Current Concepts.Indo Am. J. P. Sci, 2019; 06(11).
- Gillams K, Juliebø-Jones P, Juliebø SØ, Somani BK. Gender differences in kidney stone disease (KSD): findings from a systematic review. Current urology reports. 2021; 22:1-8.
CrossRef - Yilmaz K, Dorterler M. Characteristics of presentation and metabolic risk factors in relation to extent of involvement in infants with nephrolithiasis. Eurasian J. Med. Investig. EJMI. 2020;4:78-85.
CrossRef - Marra G, Taroni F, Berrettini A, Montanari E, Manzoni G, Montini G. Pediatric nephrolithiasis: a systematic approach from diagnosis to treatment. Journal of nephrology. 2019; 32:199-210.
CrossRef - Safdar OY, Alzahrani WA, Kurdi MA, Ghanim AA, Nagadi SA, Alghamdi SJ, Zaher ZF, Albokhari SM. The prevalence of renal stones among local residents in Saudi Arabia. Journal of family medicine and primary care. 2021; 10(2):974.
CrossRef - Moudi E, Hosseini SR, Bijani A. Nephrolithiasis in elderly population; effect of demographic characteristics. Journal of nephropathology. 2017; 6(2):63.
CrossRef - Alaya A, Sakly R, Nouri A, Najjar MF. Nutritional aspects of idiopathic nephrolithiasis in Tunisian children. Arch Ital Urol Androl. 2011;83:136-40.
- Bajrami V, Idrizi A, Roshi E, Barbullushi M. Association between nephrolithiasis, hypertension and obesity in polycystic kidney disease. Open Access Macedonian Journal of Medical Sciences. 2016;4(1):43.
CrossRef - Hallawee S. Urinary stone distribution in Samawah: Current status and variation with age and sex a cohort study. Muthanna Med J. 2015;2:93-8.
- Kittanamongkolchai W, Mara KC, Mehta RA, Vaughan LE, Denic A, Knoedler JJ, Enders FT, Lieske JC, Rule AD. Risk of hypertension among first-time symptomatic kidney stone formers. Clinical Journal of the American Society of Nephrology. 2017; 12(3):476-82.
CrossRef - Zhao A, Dai M, Chen YJ, Chang HE, Liu AP, Wang PY. Risk factors associated with nephrolithiasis: a case-control study in China. Asia Pacific Journal of Public Health. 2015; 27(2):NP414-24.
CrossRef - Saxena A, Sharma RK. Nutritional aspect of nephrolithiasis. Indian Journal of Urology: IJU: Journal of the Urological Society of India. 2010 Oct;26(4):523.
CrossRef - Shin S, Srivastava A, Alli NA, Bandyopadhyay BC. Confounding risk factors and preventative measures driving nephrolithiasis global makeup. World Journal of Nephrology. 2018;7(7):129.
CrossRef - Wigner P, Grębowski R, Bijak M, Szemraj J, Saluk-Bijak J. The molecular aspect of nephrolithiasis development. Cells. 2021 Jul 29;10(8):1926.
CrossRef - Woźniak P, Kontek B, Różański W, Olas B. The lipid peroxidation in patients with nephrolithiasis before and after extracorporeal shock wave lithotripsy. Future Medicinal Chemistry. 2018;10(23):2685-93.
CrossRef - Hadian B, Zafar-Mohtashami A, Ghorbani F. Study of urine composition of patients with recurrent nephrolithiasis in Lorestan, Iran. Iranian journal of kidney diseases. 2018;12(1):22-6.
- Grampsas SA, Chandhoke PS, Fan J, Glass MA, Townsend R, Johnson AM, Gabow P. Anatomic and metabolic risk factors for nephrolithiasis in patients with autosomal dominant polycystic kidney disease. American journal of kidney diseases. 2000; 36(1):53-7.
CrossRef - Prakash R., Arunachalam, Narayanasamy. Prevalence and socio-demographic status on kidney stone patients in Thanjavur district, Tamil Nadu, India. International Journal Of Community Medicine And Public Health. 2019; 6(5).
CrossRef - Saleem SM, Raina AF, Khan MS, Jan SS. Epidemological characteristics of urolithiasis in Kashmir division and relation to source of water. Int J Cur Res. 2015; 7(12):24450-3.
- Deshmukh SR, Khan ZH. Evaluation of urinary abnormalities in nephrolithiasis patients from Marathwada region. Indian Journal of Clinical Biochemistry. 2006; 21:177-80.
CrossRef - Ciongradi CI, Filip F, Sârbu I, Iliescu Halițchi CO, Munteanu V, Candussi IL. The Impact of Water and Other Fluids on Pediatric Nephrolithiasis. Nutrients. 2022 Oct 7;14(19):4161.
CrossRef - Nouvenne A, Meschi T, Guerra A, Allegri F, Prati B, Borghi L. Dietary treatment of nephrolithiasis. Clinical cases in mineral and bone metabolism. 2008; 5(2):135.
CrossRef - Qaseem A, Dallas P, Forciea MA, Starkey M, Denberg TD, Clinical Guidelines Committee of the American College of Physicians*. Dietary and pharmacologic management to prevent recurrent nephrolithiasis in adults: a clinical practice guideline from the American College of Physicians. Annals of internal medicine. 2014; 161(9):659-67.
- Lin Z, Lieske JC, Li Y, Jayachandran M. High water intake in preventing the risk of Uric Acid Nephrolithiasis: A systematic review and meta-analysis. Journal of Clinical Nephrology. 2019; 3(2):126-42.
CrossRef - Wang JS, Chiang HY, Chen HL, Flores M, Navas-Acien A, Kuo CC. Association of water intake and hydration status with risk of kidney stone formation based on NHANES 2009–2012 cycles. Public Health Nutrition. 2022; 25(9):2403-14.
CrossRef - Daudon M, Traxer O, Conort P, Lacour B, Jungers P. Type 2 diabetes increases the risk for uric acid stones. Journal of the American Society of Nephrology. 2006; 17(7):2026-33.
CrossRef - Dai M, Zhao A, Liu A, You L, Wang P. Dietary factors and risk of kidney stone: a case–control study in southern China. Journal of Renal Nutrition. 2013; 23(2):e21-8.
CrossRef - Boyd C, Wood K, Whitaker D, Assimos DG. The influence of metabolic syndrome and its components on the development of nephrolithiasis. Asian journal of urology. 2018;5(4):215-22.
CrossRef - Cicerello E, Ciaccia M, Cova GD, Mangano MS. The new patterns of nephrolithiasis: What has been changing in the last millennium?. Archivio Italiano di Urologia e Andrologia. 2021;93(2):195-9.
CrossRef - Rahman IA, Nusaly IF, Syahrir S, Nusaly H, Mansyur MA. Association between metabolic syndrome components and the risk of developing nephrolithiasis: A systematic review and bayesian meta-analysis. F1000Research. 2021;10.
CrossRef - Sancak EB, Reşorlu M, Akbas A, Gulpinar MT, Arslan M, Resorlu B. Do Hypertension, diabetes mellitus and obesity increase the risk of severity of nephrolithiasis?. Pakistan journal of medical sciences. 2015 May;31(3):566.
CrossRef - Gambaro A, Lombardi G, Caletti C, Ribichini FL, Ferraro PM, Gambaro G. Nephrolithiasis: A Red Flag for Cardiovascular Risk. Journal of Clinical Medicine. 2022 Sep 20;11(19):5512.
CrossRef - Shoag J, Tasian GE, Goldfarb DS, Eisner BH. The new epidemiology of nephrolithiasis. Advances in chronic kidney disease. 2015;22(4):273-8.
CrossRef - Brisbane W, Bailey MR, Sorensen MD. An overview of kidney stone imaging techniques. Nature Reviews Urology. 2016; 13(11):654-62.
CrossRef - Ulusan S, Koc Z, Tokmak N. Accuracy of sonography for detecting renal stone: comparison with CT. Journal of Clinical Ultrasound. 2007; 35(5):256-61.
CrossRef - Kalaitzidis RG, Damigos D, Siamopoulos KC. Environmental and stressful factors affecting the occurrence of kidney stones and the kidney colic. International urology and nephrology. 2014; 46:1779-84.
CrossRef

This work is licensed under a Creative Commons Attribution 4.0 International License.





