How to Cite | Publication History | PlumX Article Matrix
Impact of Pharmaceutical Care Interventions on Clinical outcome in Patients with Hypertension
Haneena1* , Neehara Bijal K1
, Neehara Bijal K1 , Aswin Krishna VV1
, Aswin Krishna VV1 , Ahammed Shameem P1
, Ahammed Shameem P1 , Thangamani S1
, Thangamani S1 and Kiran DR2
and Kiran DR2
1Department of Pharmacy Practice, Grace College of Pharmacy, Palakkad, Kerala, India.
2Medical Superintendent, Karuna Medical College Hospital. Palakkad Kerala. India.
Corresponding Author E-mail: haneenaneenu9809@gmail.com
DOI : http://dx.doi.org/10.13005/bbra/3223
ABSTRACT: Background: Hypertension poses a serious threat to public health being a common and challenging condition to treat. The main cause of poor blood pressure regulation is non-adherence to treatment. Enhancing patient compliance and promoting preventative care are two benefits of pharmaceutical care based on patient education. Objective: The study was aimed to evaluate the therapeutic outcome of different class of antihypertensive after pre and post intervention in hypertensive patients and to evaluate whether patient participation in a pharmaceutical care program is associated with reduction in blood pressure. Method: A 6-month hospital based prospective interventional study was performed with 125 patients in the outpatient department of general medicine. The patients' medical records were reviewed and recorded the initial Blood pressure according to which pharmaceutical care intervention was performed which included verbal counselling, patient information leaflets, and patients were divided according to which they receive monotherapy and combination therapy then subsequent monitoring with two Follow-ups were carried out over a one-month interval and assessed the changes in Diastolic blood pressure and Systolic blood pressure. Result: Pharmaceutical care intervention provided to the patients, resulted in improvement in Blood pressure control knowledge and adherence to medication. Pharmaceutical care's impact on Systolic blood pressure and Diastolic blood pressure in patients undergoing monotherapy Angiotensin receptor blockers significantly reduced blood pressure readings, and in patients receiving combination therapy, angiotensin receptor blockers plus beta blockers significantly decreased systolic blood pressure while angiotensin receptor blockers plus calcium channel blockers significantly decreased diastolic blood pressure. Conclusion: Hypertensive patients who received pharmaceutical care reported better blood pressure management and overall patient satisfaction.
KEYWORDS: Blood pressure; Clinical outcome; Hypertension; Monotherapy; Pharmaceutical care
Download this article as:| Copy the following to cite this article: Haneena H, Bijal K. N, Krishna V. V. A, Shameem P. A, Thangamani S, Kiran D. R. Impact of Pharmaceutical Care Interventions on Clinical outcome in Patients with Hypertension. Biotech Res Asia 2024;21(1). |
| Copy the following to cite this URL: Haneena H, Bijal K. N, Krishna V. V. A, Shameem P. A, Thangamani S, Kiran D. R. Impact of Pharmaceutical Care Interventions on Clinical outcome in Patients with Hypertension. Biotech Res Asia 2024;21(1). Available from: https://bit.ly/48E14Qh |
Introduction
Systolic blood pressure (SBP) and diastolic blood pressures (DBP) that are elevated above the normal range [140/90mmHg] are referred to as hypertension (HTN).1 Blood pressure (BP) is the measure of the force that blood exerts against the walls of arteries. Pumping blood out of the heart is more difficult when pressure is high. 2 Many people now have HTN, especially in low- and middle-income nations (LMICs). According to estimates, 1.39 billion persons globally had HTN in 2010.3 Excessive salt consumption, Obesity, alcohol use, inactivity, and unhealthy eating and low potassium consumption are risk factors for HTN.
Treatment decisions for hypertension focus more on overall vascular risk factors than just blood pressure. 4 Initial HTN treatment should focus on lifestyle management, which includes dietary treatments (such as lowering salt and boosting potassium), alcohol avoidance, multifactorial diet control, weight loss, quitting smoking, exercising regularly, and stress management. 5 Pharmaceutical care (PC) designed to increase patient’s adherence to (antihypertensive) medicines. Along with PC responsible pharmacological therapy is provided with the goal of attaining specific results that improve a patient’s quality of life. 6 Patient compliance can increase by up to 100% with pharmaceutical care (PC) based on patient education. PC increased the percentage of patients with acceptable blood pressure from 54.0% to 98.0%. 7 The management of prevalent clinical diseases is the primary emphasis of PC and a good example of managing a chronic illness is HTN. PC gives consideration to issues with pharmacological therapy (patient compliance, identification of side effects, dosage optimization) can be expected to improve outcomes. 8
The lack of effectiveness of anti-hypertensive therapy is caused by both patient-related factors, such as non-adherence, and factors related to the health care system and medical staff (for example, lack of access to medical care). Therefore, through PC intervention can improve the Cooperation between physicians, pharmacists, and other medical personnel, as well as encouraging patient to systematic control of BP results in improvement of hypertension. 9
PC is one of the strategies that involve interacting with patients and offering counselling about their condition and medications in order to increase patient adherence to therapy. 10 The primary goal of PC is to determine whether a patient’s involvement in a PC programme is linked to a drop in BP, an improvement in quality of life (QOL), and better medication-taking habits. 11
Patient information leaflet (PIL) is one of the patient counselling techniques Included in PC. PIL is necessary since patients were unable to control their illnesses because they did not have access to the information they needed. 12,13 PIL contains details in simple language that patients can understand. PIL is an important teaching tool in patient counselling. 14,15 So this study was aimed to evaluate the impact of pharmaceutical care interventions on clinical outcome in patients with hypertension.
Materials and Methods
A 6 month hospital based prospective interventional study was performed with 125 patients (selected based on study criteria) in the outpatient department of general medicine at Karuna Medical College Hospital in Palakkad, Kerala, from October 2021 to March 2022.The patients who were eligible for inclusion in our study were previously diagnosed with HTN and are taking antihypertensive (both monotherapy and combination therapy) with or without co morbidities like diabetes, dyslipidaemia, hypothyroidism, coronary artery disease, and myocardial infarction. The exclusion criteria included newly diagnosed hypertensive patients, pregnant and lactating women, patients with co morbidities such as chronic kidney disease, cancer, stroke, COPD who refused to provide written information consent, patient who was not interested to participate in the PC and if the dose is changed during the study period. Selected patients divided based on the medications they have given with the same dose in each group.
Patient’s data collected with predesigned data entry form including demographic information like age, sex, social habits, co-morbidities, SBP, DBP and antihypertensive for treating hypertension. The PC program which include patient counselling have given to the patients who are willing to participate the patient counselling programme and developed a PIL according to the individual patient’s need which included initial baseline information such as patient age, sex, co-morbid condition, BP value, physical activities, food habits, social habits, salt intake and adherence to their individual antihypertensive medications. Prepared PIL was provided as a visual reminder to the patient. PC grounded in patient education can improve patient compliance to drug therapy. After the PC intervention done two follow-ups in every month and changes in BP were recorded respectively.
Through the two follow ups checked that the patient is properly following the medication ie; proper dose and duration and change in BP is recorded. By comparing the current SBP and DBP (BP value of 2nd follow up) value with the baseline SBP and DBP (before the PC programme) the percentage mean change (Percentage mean change refers to the average percentage difference in blood pressure readings before and after the intervention) in SBP and DBP for monotherapy and combination therapy were calculated to assess the clinical outcome for the PC provided.
The data was entered into Microsoft Excel 2007 and examined using graph pad prism. ANOVA [One way] is used to compare continuous variables’ baseline and follow-up values. Significant was defined as a p value of <0.05 which means A p-value of less than 0.05 indicates that the results are statistically significant, meaning the observed changes are unlikely due to chance.
Result
A total of 125 participants were included to determine the pharmaceutical care interventions affected the therapeutic outcome of hypertensive patients. Female were shown to be more frequently affected 58.4% of the time when analysed by sex (table 1). According to the age distribution of the population being studied, out of 125 study participants, most of the hypertension patients were above 50years. (Table1). The therapy wise distribution revealed that more patients (59.2%) were receiving monotherapy than combination therapies (40.8%) (Figure1). Effectiveness of PC in reducing BP was achieved by resolving and preventing drug therapy problems (missing daily doses, unaware about the importance of therapy, inappropriate adherence) with regular monitoring and counselling the patient.
In monotherapy reduction in SBP was evaluated in review 2 (Table 2), in this Angiotensin receptor blockers (ARBs) shows significant difference (P=.05) the percentage mean change is 7.19%, followed by Calcium channel blocker (CCBs) (3.54%), Diuretics (DIU) (2.06%), and Beta blockers (BB) (2. 05%).In DBP ARBs have a percentage mean change of 6.31% with a (P=.05) making them significantly more successful than other antihypertensive like CCBs, BBs, and DIU, which had percentage mean changes of 5.01%, 3.23%, and 2.94%, respectively (Table 2).
In combination therapy ARB+BB (n=10) was found to be the most significant in reducing SBP with a percentage mean change of 9.35%, and a (P=.05). Other combinations, such as ARB+DIU and ARB+CCB showed no significant reduction of SBP, DBP among the study population with percentage mean changes of 6.92% and 2.93%, respectively (Table3). No drug combination was shown to significantly lower DBP when used in combination with the other medications that were employed, according to the measurement of DBP. From these BP reduction values we assessed the clinical outcome before and after the PC implementation.
Table 1: baseline characteristics of study population.
| S. No | Parameters | No of Patients (n=125) | Percentage of Patients (%) |
| 1. | Sex | ||
| Female | 73 | 58.4 | |
| Male | 52 | 41.6 | |
| 2. | Age (years) | ||
| <40 | 9 | 7.2 | |
| >40 | 8 | 6.4 | |
| ≥50 | 106 | 84.8 | |
|
3. |
Co morbid disease | ||
| Coronary artery disease | 7 | 5.6 | |
| Type 2 DM | 42 | 33.6 | |
| Hypothyroidism | 5 | 4 | |
| Dyslipidaemia | 5 | 4 | |
| 4. | Risk factors | ||
| Smoker | 42 | 33.6 | |
| Alcoholic | 36 | 28.8 | |
| Smoker + Alcoholic | 25 | 20 | |
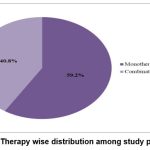 |
Figure 1: Therapy wise distribution among study population |
Table 2: Effect of pharmaceutical care on SBP and DBP in Hypertensive Patients used as Monotherapy
| Parameters | Baseline | Review I | Review II | Percentage mean change (%) | P value | |
| ARB(n=33) | ||||||
| SBP | 142.12 ±13.42 | 137.57±13.93 | 131.9±10.56 | 7.19 | 0.008* | |
| DBP | 88.78±9.13 | 84.8±8.97 | 83.1±7.84 | 6.31 | 0.019* | |
| BB(n=9) | ||||||
| SBP | 135.55±13.42 | 133.11±9.04 | 132.77±10.82 | 2.05 | 0.846 | |
| DBP | 86.66±8.16 | 84.33±7.96 | 83.8±7.2 | 3.23 | 0.711 | |
| CCB(n=23) | ||||||
| SBP | 141.00±15.77 | 138.3±12.9 | 136±11.3 | 3.54 | 0.454 | |
| DBP | 86.86±12.29 | 84.43±11.5 | 82.5±10.6 | 5.01 | 0.450 | |
| DIU(n=7) | ||||||
| SBP | 145.71±19.16 | 146.42±15.74 | 142.14±8.39 | 2.06 | 0.847 | |
| DBP | 84.8±11.6 | 83.2±13.9 | 82.3±10.2 | 2.94 | 0.925 | |
(* Statistically significant p<0.05)
Table 3: Effect of pharmaceutical care on SBP and DBP in Hypertensive Patients used as Combination therapy
| Parameters | Baseline | Review I | Review II | Percentage mean change (%) | P value |
| ARB+DIU(n=24) | |||||
| SBP | 144.83±16.65 | 138.63±13.76 | 134.8±12.32 | 6.92 | 0.061 |
| DBP | 89.29±13.30 | 85.78±11.28 | 83.37±10.7 | 6.63 | 0.224 |
| ARB+CCB(n=13) | |||||
| SBP | 145.57 ±20.44 | 142.46±16.2 | 141.3±15.8 | 2.93 | 0.822 |
| DBP | 90.57±13.72 | 85.92±12.13 | 80.71±12.22 | 10.8 | 0.158 |
| ARB+BB(n=10) | |||||
| SBP | 160.30±10.37 | 153.5±9.2 | 145.3±8.4 | 9.35 | 0.005* |
| DBP | 94.10±14.98 | 90±12.64 | 89.20±12.6 | 5.20 | 0.677 |
(* Statistically significant p<0.05)
Discussion
Patients with hypertension participated in a prospective interventional study to evaluate the therapeutic effectiveness of various antihypertensive classes before and after the intervention. In this study, the majority of the hypertension patients were above the age of 50. Due to the fall in oestrogen levels associated with menopause, women are demonstrated to be affected more frequently than men (41.16% vs. 58.4%), although oestrogen replacement therapy does not lower BP or lower the incidence of hypertension in women. 16,17
One of the findings is that patients who get monotherapy have greater rates (59.2%) than those who receive combination therapy (40.8%). The patient baseline data were obtained after enrolling patients in the study and delivering pharmaceutical care, and then BP was noted after one month of follow-up and again after one month of follow-up, and these values were analysed to find the effectiveness of pharmaceutical care in reducing SBP and DBP in monotherapy. Due to more primary care appointments and fewer emergency consultations, the PC programme has improved the care profile for hypertension patients. 18 It was discovered that ARBs are having more efficacies in lowering the BP along with Pharmaceutical care. 19,20
Out of 51 patients getting combination medication, those using ARB+BB (n=10) were found to be the most effective at lowering SBP in the study population, and their percentage mean change of 9.35% had a (P<0.05) indicating that it is significant in comparison to other studies. It shows that the use of CCB and ARB together is an acceptable antihypertensive strategy. 21 The choice of combination therapy is based on the risk factors, the existence of comorbidities, and is individualized for each patient. 22, 23 Similarly it was found that no drug combination significantly decreased DBP. The percentage mean change for ARB+CCB is 10.8% (0.158), whereas ARB+DIU’s change is 6.63% (0.244), and ARB+BB’s change is 5.20%. (0.677). ARB and amlodipine’s higher efficacy and tolerance have been shown in several studies. 24, 25 These outcomes were achieved by providing patient counselling on lifestyle modifications (reduced salt and pickle intake, regular physical activity) along with drug therapy. This study finding shows that providing hypertensive patients with pharmaceutical care can improve in BP management and as a result reduce the risk of hypertension-related complications.
Limitations
In this study we could measure the clinical outcome only by reduction in BP
Here we selected previously diagnosed hypertensive patients so we can’t include control group for the study
In a 6 month study only who are willing for PC programme only included in study.
There is more chance of getting bias in terms of medication intake of patient this would affect the result.
Conclusion
This study finding demonstrated that hypertensive patients receiving antihypertensive shows significant reduction in their BP values as a result of pharmaceutical care. There is a significant change in BP value before and after the intervention. Through the antihypertensive medication along with the PC can control the BP and improve the quality of life of patient.
Acknowledgement
We would like to thank Dr. Kiran D R MD, Department of General Medicine, Karuna Medical College, Vilayodi, Chittur, Grace college of Pharmacy and all the patients who participated in the study.
Conflict of Interest
Here we would like to declare that we don’t have any conflict of interest.
Funding Sources
Here we would like to declare that we don’t have any funding sources used.
References
- Smitha VK, Chand S, Nandakumar UP, Joel J, Sharma R. Pharmacoeconomic evaluation of antihypertensive therapy. BBRC. 2021;14(2):112-117.
- Parveen R, Rao M VP. Evaluating the cost effectiveness of different groups of hypertension therapy: A pharmacoeconomic study. AJPCR. 2018;11(4):200.
CrossRef - Mills KT, Stefenescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020; 16(4):223-237.
CrossRef - John NN, Krishnan R, Midhun JV, Juan R. A study to evaluate Pharmacoeconomics of antihypertensive drugs in a tertiary care teaching hospital. Journal of drug delivery & therapeutics. 2010;10(4-s):176-180. http://dx.doi.org/10.22270/jddt.v10i4-s.4227
CrossRef - Nicoll R, Henein MY. Hypertension and life style modification: how use full are the guidelines. BJGP. 2010;60(581):879-880. DOI: 10.3399/bjgp10X544014
CrossRef - Arabadzieva D, Petkova V, Csollei M, Dimitroe MV. Pharmaceutical care approach and hypertension. European journal of pharmaceutical medical research. 2015;2(3)784-795.
- Garcao JA, Cabrita J. Evaluation of pharmaceutical care program for hypertensive patients in rural Portugal. Journal of APA. 2002;42(6):44-50.
CrossRef - Oparah CA, Adje DV, Enato FE. Outcomes of pharmaceutical care intervention to hypertensive patients in a Nigerian communitypharmacy. IJPP. 2006;14:115-116.
CrossRef
- Castro MSD, Fuchs FD, Santos MC, Maximiliano P, Gus M et al., pharmaceutical care program for patients with uncontrolled hypertension. AJH. 2006;19:528-533.
CrossRef - Beney J, Bero L, Bond CM. expanding the roles of outpatient pharmacists: Effects on health services utilisation, costs and patient outcomes. Cochrane data base of systematic review. 2000;4(2)13-16.
CrossRef - Martins BPR, Aquino AT, Provin MT, Lima DM, Dewlf NLS. Pharmaceutical care of hypertensive patients provided within the family health strategy in Goiana, Brazil. BJPS. 2013;48(3):609-618.
CrossRef - Adepu R, Swami MK. Development and evaluation of patient information leaflets (PIL) usefulness. Indian journal of pharmaceutical science. 2012;22(4):16-25.
CrossRef - Lampert A, Wien K, Haefeli W E, Seidling HM. Guidance on how to achieve comprehensible patient information leaflets in four steps. International journal for quality in health care. 2016;28(5)634-638
CrossRef - Owusu FWA, Yedoah GN, Aboagye RA, Amengor CDK, Entsie P. The role of the patient information leaflet in patients’ medication therapy: A case study within the Kumasi metropolis of Ghana. The scientific world journal. 2020;24(5):125-132.
CrossRef - Adepu R, Nagavi BG. Patient information leaflets design and Readability. Pharma Rev. 2003; 2:135-43.
- Osude N, Arvizu RD, Markossian T etal., Age and sex disparities in hypertension control: The multy-ethnic study of atherosclerosis (MESA). ASPC. 2021; 8:1-7.
CrossRef - Chowdhery EK, Owen A, Krum H,Wimg LM et al., Barriers to achieving blood pressure treatment targets in elderly hypertensive individuals.J Hum Hypertens. 2013;27:545-551.
CrossRef - Etemad LR, Hay JW. Cost-effectiveness analysis of pharmaceutical care in a medicare drug benefit program. MDMC. 2003;6:12-18.
CrossRef - Abraham H M A, White CM, White WB. The comparative efficacy and safety of angiotensin receptor blockers in the management of hypertension and other Cardiovascular diseasaes. PMC. 2015;38(1):33-54.
CrossRef - Neto PRO, Marusic S, Guidoni CM, Baldoni AO, Renovato RD et al., Economic evaluation of pharmaceutical care program for elderly diabetic and hypertensive patients in primary health care. JMCP. 2014;21(1):66-75.
CrossRef - Oparil S, Weber M. Angiotensin receptor blocker and dihydropyridine calcium channel blocker combinations: an emerging strategy in hypertension therapy. Postgrad Med.2009; 121(2):25-39.
CrossRef - Karla S, Karla B, Agarwal N. Combination therapy in hypertension: an update.
Diabetology and Metablic Syndrome. 2010;2(44):2-11.
CrossRef - Norris K, Neutel JM. Emerging Insights in the First-Step Use of Antihypertensive Combination Therapy. J Clin Hypertens (Greenwich). 2007;9(12 Suppl 5):5-14.
CrossRef - Kim HS, Ryu KH, Lee NH, Kang JH, Kim WS. Efficacy of fixed dose amlodipine and losartan combination compare with amlodipine monotherapy in stage II hypertension: a randomised, double blind, multi-center study. BMC Research Notes. 2011;4:461-468.
CrossRef - Gupta R, Guptha S. Strategies for initial management of hypertension. Indian J Med Res. 2010;132:531-542.

This work is licensed under a Creative Commons Attribution 4.0 International License.





