Manuscript accepted on : September 04, 2009
Published online on: 28-12-2009
Afeyodion Akhator1 and Clement Osime2
1Department of Surgery, Faculty of Clinical Medicine, College of Health Sciences, Delta State University, Abraka, Delta State, Nigeria
2Department of Surgery, University of Benin, Teaching Hospital, Benin City, Nigeria
Corresponding Author E-mail: clementosime@yahoo.com.
ABSTRACT:
KEYWORDS: Bowel resection; Colocolonic intussusception
Download this article as:| Copy the following to cite this article: Akhator. A, Osime. C. Colocolonic Intussusception in an Adult Being Prepared for Bowel Resection - A Rare Form of Presentation. Biosci Biotechnol Res Asia 2009;6(2) |
| Copy the following to cite this URL: Akhator. A, Osime. C. Colocolonic Intussusception in an Adult Being Prepared for Bowel Resection - A Rare Form of Presentation. Biosci Biotechnol Res Asia 2009;6(2). Available from: https://www.biotech-asia.org/?p=8713. |
Introduction
Intussusception entails the telescoping of one part of the intestine into another part; usually from proximal to distal segment. Intussusception occurs commonly in children where it is more an ileocolic intussusception and more likely of a benign aetiology and without a lead point. Adult intussusception on the other hand is usually of the colocolonic type and it is often associated with a lead point. In most cases, the lead point is a malignant growth1. The presentation of adult intussusception is usually of insidious onset with recurrent symptoms of partial intestinal obstruction2. Some of the precipitating factors for intussusception include diarrhea and constipation. Diarrhea is believed to cause intussusceptions by its associated vigorous and disturbed peristalsis3. Soap and water enema may also initiate vigorous peristalsis by irritating the intestine. To the best knowledge of the authors, there has not been reports that showed intussusception in a patient with colonic tumour who developed signs of acute intestinal obstruction secondary to intussusception shortly after receiving soap and water enema. We present a case of colocolonic intussusception that presented acutely in a patient with colonic tumour soon after soap and water enema given as part of preoperative preparation for a right hemicolectomy.
Case Report
Mr. O.O. a known hypertensive presented to the surgical outpatient on 30/07/08 with a 15 month history of recurrent passage of bright red blood per rectum. The bleeding was usually mild but the index episode was severe enough to have precipitated a syncopal attack necessitating his referral to our center. There was associated alteration of bowel habit with spurious diarrhea of mucus and blood alternating with constipation. The patient also had colicky lower abdominal pain, weight loss and anorexia. Patient consumed alcohol occasionally for 20years and smoked 1-2 sticks of cigarette for 10 years. There was no family history suggestive of colorectal tumours.
Examination at presentation revealed an asthenic man, mildly dehydrated and pale. Abdominal examination was unremarkable, rectal examination revealed no signs of haemorrhoids. Gloved finger was stained with bright red blood.
Barium enema showed a constant space occupying lesion in the transverse colon, between the proximal 2/3 and distal 1/3. Packed cell volume was 44%. Patient was counseled for surgery, and bowel preparation began with low residue diet, soap and water enema, and oral antibiotics.
Two days after commencement of soap and water enema, the patient suddenly developed colicky abdominal pains with vomiting of recently ingested meals. Abdominal examination showed visible peristalsis. An assessment of acute intestinal obstruction was made. Patient was resuscitated with intravenous fluids and was taken in for emergency laparotomy.
Findings at surgery were colocolonic intussusception involving distal 1/3 of the transverse colon into the descending colon. The apex of the intussusceptum was a cauliflower growth in the transverse colon measuring 4 x5cm. There were 2 small nodules in the greater omentum. An extended left hemicolectomy and end to end anastomosis was done between the transverse colon and the sigmoid colon.
Patient had an uneventful post operative course; sutures were removed on the 10 and 11th day and discharged home on the 12th post operative day. Histology was an adenocarcinoma of the colon. He subsequently had 6 courses of 5 fluorouracil and has remained symptom free.
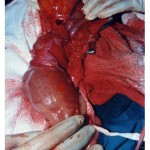 |
Figure 1
|
Discussion
Intussusception occurs when a loop of intestine (intussusceptum) telescopes into an adjacent segment (intussuscepiens). Adult intussusception is a rare condition and accounting for 1% of all cases of adult intestinal obstruction4. In adult intussusception cases, 38-45% occurs in the colon and 52-55% in the small intestine5. The lead point in colocolonic intussusception is usually neoplastic and 50-60% is malignant6.
The symptoms of colocolonic intussusception in adults are usually that of chronic intestinal obstruction, and not one of acute intestinal obstruction2. Our patient going into acute intestinal obstruction during bowel preparation for colonic resection may be due to the increased and disturbed peristalsis induced by the bowel preparation forcing the tumour to act as a lead point telescoping the distal transverse colon into the descending colon.
It is difficult to diagnose intussusception in an adult preoperatively; most cases are diagnosed at laparotomy for intestinal obstruction. Radiological features of intussusception have been described1. These were not useful in our case because the sudden onset of acute intestinal obstruction in a patient with colonic tumour and surgery had to be done urgently without further diagnostic investigations.
Treatment for adult intussusception due to malignancy is radical resection; reduction of the intussusception should be avoided since it can cause bowel perforation and tumour dissemination7. In emergency cases, the surgeon has to decide between resection with immediate or delayed anastomosis and colostomy with a deferred resective treatment2. We were able to perform a one stage resection and anastomosis in our case because patient was already being prepared for the surgery.
In conclusion, we presented a case of colocolonic intussusception in a patient with colonic tumour. We believe the intussusception was induced by the bowel preparation and recommends immediate surgery for similar cases.
References
- Jaremko JL, Rawat B. Colo-colonic intussusception caused by a solitary Peutz-Jegher’s polyp. The British Journal of Radiology2005;78: 1047-1049. doi: 10.1259/bjr/25000606.
- Yol S, Bostanci EB, Ozogul Y, Akoglu M. Extensive adult colo-colonic intussusception from ascending colon to sigmoid colon: Report of a case. Turk J Gastroenterol 2004; 15(3): 201-203.
- Chia AA, Chia JK. Intestinal intussusceptions in adults due to acute enterovirus infection. J Clin Pathol Published online 30 July 2009. Doi 10.1136/jcp2008.063610.
- Law HL, Aldrete JS. Small bowel obstruction: a review of 465 cases. South Med J 1976; 69: 733-734.
- Schuid Y, Van Gansbeke D, Ansay J. Intussusception in adults. Acta Chir Belg 1985; 85(1): 55-60.
- Lorenzi M, Iroatulam AJ, Vemillo R et al. Adult colonic intussusception caused by malignant tumour of the transverse colon. Am Surg 1999; 65(1): 11-14.
- Yakan S, Caliskan C, Makay O et al. Intussusception in Adults: Clinical characteristics, diagnosis and operative strategies. World J Gastroenterol 2009; 15(16): 1985-1989. Doi: 10.3748/wjg.15.1985

This work is licensed under a Creative Commons Attribution 4.0 International License.





