How to Cite | Publication History | PlumX Article Matrix
Salman Yousuf Guraya
Department of Surgery, Taibah University Almadinah Almunawwarah Saudi Arabia. Corresponding Author E- mail: salmanguraya@gmail.com
DOI : http://dx.doi.org/10.13005/bbra/2340
ABSTRACT: Clinical reasoning (CR) is considered to foster clinical practice and competence. However, very few faculty development programs are available that can enhance the faculty’s expertize in this innovative educational strategy. This study aims at elaborating the core concepts of teaching and assessing CR that can equip medical faculty with the desired knowledge and competence.The databases of ISI web of knowledge, MEDLINE, the Cochrane Library, and EBSCO were searched for the full-text English-language articles published during 2000 to 2015 using Medical Subject Headings (MeSH) keywords “Clinical reasoning” AND “Meta-cognitive” OR “Flipped classroom” OR “Work-place based assessment” OR “Clinical competence” OR “ Experiential learning” AND “Debrief”. Initial search showed 771 articles. Further search on the bibliographic list and exclusion of non-relevant material finalized 58 articles for this systematic review. The body of literature has shown that teaching CR challenges the learner to manage a given case by data acquisition, diagnostic solutions, and dual processing of information in an integrated and cohesive learning environment. Several educational strategies are employed; metacognition, deliberate practice, experiential learning, and clinical debrief using a flipped classroom model in a blended learning approach. Due to multi-dimensional and context-specific characteristics of CR. assessment of this domain is challenging. Several assessment tools such as multiple choice and extended matching questions, script concordance test, long case examination, mini-CEX, and portfolios are shown to have the desired reliability and validity to assess CR skills. Literature has shown an encouraging trend towards the faculty acquisition of clinical reasoning skills that requires careful scaffolding of this domain throughout the curriculum. A myriad of instructional strategies and assessment modalities are used in developing CR skills. Faculty development programs should train the faculty in enhancing the desired expertize for teaching and assessing CR skills.
KEYWORDS: Clinical reasoning; Meta-cognitive; Thematic case discussion; Flipped classroom; Experiential learning; Debrief; Work-place based assessment
Download this article as:| Copy the following to cite this article: Guraya S. Y. The Pedagogy of Teaching and Assessing Clinical Reasoning for Enhancing the Professional Competence: A Systematic Review. Biotech Res Asia 2016;13(3). |
| Copy the following to cite this URL: Guraya S. Y. The Pedagogy of Teaching and Assessing Clinical Reasoning for Enhancing the Professional Competence: A Systematic Review. Biotech Res Asia 2016;13(3). Available from: https://www.biotech-asia.org/?p=16521 |
Introduction
Clinical reasoning (CR) implies an organized and analytical strategy that integrates all relevant information in the quest for the best diagnosis and therapy for individual patients (1). CR has been defined as “the ability to integrate and apply different types of knowledge, to weigh evidence, critically think about arguments and to reflect upon the process used to arrive at a diagnosis” (2). Academics agree that CR is pragmatic to its core content and differs from expert opinion that is a hallmark of evidence-based medicine (3). In CR, the clinical decision making envisages an individual’s capabilities to imagine all that is possible and to critically evaluate the likelihood and significance of one outcome over the other (4). This teaching strategy integrates complex cognitive process with meaningful interpretation of patients’ problems leading to an effective management plan for the case under consideration. The acquisition of CR skills facilitates collaborative learning and critical thinking and fosters the ethical domains of medical professionalism (5) (6).
Academics have proposed that the skills of CR must be developed during the early years in medical training and be further refined during subsequent years (7) (8). Literature has shown that diagnostic errors in medicine may occur in 5-15% of cases and two-thirds of these are cognitive errors due to flaws in decision making and diagnostic reasoning (9). Deeper understanding and meta-cognitive analysis involved in the acquisition of clinical reasoning skills have the potential of eliminating cognitive errors. Nevertheless, a body of literature has argued about the complex nature of CR due to several pre-requisites (10); sound and content-specific knowledge that is organized in memory as frameworks of symptoms and findings for a given diagnosis known as instance scripts (11), a range of working solutions for a given clinical problem and a tolerance for ambiguity (12), and reflective understanding of clinical practice (13).
Despite its complexity, the knowledge of how clinicians reason the disease process has exceptionally advanced but the evolution of faculty training process that can train the faculty about how to reason has been limited (14). One barrier may be the limited knowledge translation about CR from literature to the busy faculty. “Clinical teachers need to understand their own clinical reasoning processes as well as be able to convey that knowledge to their trainees. At the same time, they need to understand the developmental stages of clinical reasoning and be able to nurture each trainee’s own expertise” (15). Literature shows a scarcity of well-structured faculty development programs that can enhance the faculty’s expertize about this innovative educational strategy. This systematic review aims at providing a holistic view of the teaching pedagogies and assessment tools in CR with an attempt to bridging the gaps in knowledge that may help accomplish effective professional development of the medical faculty.
Study Design and Methodology
During May 2016, this systematic review was conducted by searching the databases of ISI web of knowledge, MEDLINE, the Cochrane Library, and EBSCO for the full-text English-language articles published during 2000 to 2015. This systematic review rigorously followed the guidelines by Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (16). Medical Subject Headings (MeSH) keywords “Clinical reasoning” AND “Meta-cognitive” OR “Flipped classroom” OR “Work-place based assessment” OR “Clinical competence” OR “Experiential learning” AND “Debrief” were used for literature search. All peer reviewed review articles including meta-analysis and systematic reviews and original research including longitudinal and cross sectional studies using quantitative/qualitative/ mixed method studies were included in this search. Main purpose of this search was aimed at finding the evidence for best available teaching and assessment tools for CR. Personal opinions, short communications, editorials, and conference proceedings were excluded. Initial search showed 771 articles in the bibliographic list. Review of bibliographic list of all retrieved articles was further refined that showed several non-relevant material such as abstracts, conference proceedings, letters to editor, and short communications. These publication categories were excluded. Finally, 58 articles were selected for this systematic review. Figure 1 illustrates a flow diagram that shows the systematic selection of articles in this search.
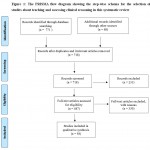 |
Figure 1: The PRISMA flow diagram showing the step-wise schema for the selection of studies about teaching and assessing clinical reasoning in this systematic review
|
Key Search Findings and Thematic Analysis of Results
A wealth of literature shows a distinct trend towards the incorporation of teaching and assessing CR in medical curricula. The themes derived from this search are clustered in appropriate headings and an integrated account about various dimensions of CR is provided in the later sections of this article.
The Pedagogy of Teaching Clinical Reasoning
Models for teaching clinical reasoning
Traditional CR sessions include a myriad of strategies that incorporate clinical case presentations, case based discussions, clinical problem solving exercises, chart stimulated recall, and structured case presentations. Several models for teaching CR have been described, but the two most popular models of SNAPPS (17) and One Minute Preceptor (OMP) (18) are elaborated in Table 1.
Table 1: The SNAPPS and OMP models for teaching clinical reasoning
| SNAPPS (17) | One Minute Preceptor (18) |
| Summarise the case
Narrow the differential diagnoses Analyse the differentials Probe the preceptor about uncertainties Plan patient management Select case-related issues for self-study |
– Student presents a case
– Students is asked to make a diagnosis – Students is probed for the diagnosis – Preceptor teaches about; · General principles · Principles of management · Key communication skills |
The SNAPPS model promotes the expression of intuitive and analytical thinking and promotes self-reflection by the learners; whereas the OMP model motivates the learner to suggest and justify the diagnosis by applying appropriate CR skills. Both SNAPPS and OMP have the mandatory component of formative assessment of the learners. During the process of CR, learners should be encouraged to utilize the given epidemiological data such as seasonal, geographical or cultural characteristics of illnesses that can help them in narrowing down the diagnosis (19). Learners should also prioritize and shortlist from a range of differential diagnoses in a given context, emphasizing certain points in favour and against each diagnosis. They should be able to demonstrate how they arrived at a particular conclusion (20).
The desired core domains required from the learners during the acquisition of CR skills include; Metacognition and reflection where learners are encouraged to think about what they could be missing and are given the chance to reflect on their diagnostic approach (21) (22), and deliberate practice that provides “opportunities for repeated practice, requesting honest feedback on performance at frequent intervals, maximizing learning from each case, reflecting on feedback and errors to improve performance and using mental practice to support clinical experiences” (23).
Thematic case discussions
A typical CR module integrating thematic case discussion starts with online introduction of a carefully drafted case script about a disease or a group of clinical conditions. The script of cases demand increasingly complex problem solving, guided by their stage of learning (novice, advanced beginner, competent and proficient practitioner and expert) (24). The students are then involved in online learning and they expand their knowledge-base by reading the provided online resources. They may be provided with additional videos, simulated scenarios and short lectures to complement the course material. The entire exercise has been shown to enhance self-direct learning and critical thinking (25). At the end of this week, students will report to their designated hospitals for the transfer of their knowledge to a patient in real clinical environment.
The flipped classroom
The illustrated model is based on the philosophy of the flipped classroom where learner is assigned pre-class content for reading and understanding and then the class time is used for the application of knowledge in an active learning environment (26). Pre-class content may be short videos, didactic lectures, course material and may include animation with narration and text (27). Such teaching approaches employ active and self-directed learning and lead to positive learning outcomes (28). “The flipped classroom model has been described as particularly well suited for medical education, as the pre- class assignment can create a framework of core knowledge, and the active learning exercise can then embed the knowledge in an interactive, compelling and engaging format” (29). The flipped classroom has been shown to be a promising platform for making more efficient use of students’ time, and for enhancing their satisfaction with the necessary didactic learning of the clerkship (30). However, a study by Missildine et al. conducted on nursing students randomised to a flipped classroom teaching model, showed that the student satisfaction was lower with the flipped classroom model than with didactic teaching strategies (31).
The instructional strategies employed during the teaching of clinical reasoning
CR integrates a range of cognitive processes where a learner gathers information about a given case, synthesises that information using knowledge-based approaches and then draws a treatment and management strategy (24). The framework of instructional strategies used in CR envisages to embed the cognitive principles that can help promote contextual learning. A brief account of each instructional strategy is detailed as under.
Themed case discussion
involves a weekly online introduction of a new theme to the learners. Each theme contains a group of similar conditions and will require the learners to study the provided material, to search for new resources to explain and consolidate cognition, and to interact with patients in a given clinical environment (32). This exercise may bring new emerging themes that will be elaborated and clarified in an integrated manner. However, the entire discussion and learning process will revolve around the patient-centred learning strand, contextualised to the primary theme. Such meta-cognitive process integrating enquiry and discussion promotes engagement with relevance to clinical practice (33).
Patient-centered consultation, a key strand in CR pedagogy, promotes respect for patients, enhances communication skills, and contributes to successful patient management (34). Medical educators have stressed the need to encourage the learners to adopt a patient-centred learning approach right from the start of their clinical exposure (35) (36). Usherwood et al. reported that students’ consulting skills improved during a general practice based interviewing course and proposed that embedding such a course in curriculum would be helpful in enhancing their clinical competence (37). Nevertheless, the available body of literature lacks clarity over the precise definition, the tools for accurate measurement, and the relationship between patient-centred care and patient outcomes.
Experiential learning refers to “the process whereby people individually and in collaboration with others, engage in direct encounter and then purposefully react upon, validate, transform, give personal meaning to and seek to integrate their different ways of knowing” (38). Experiential learning and reflective practice forums are shown to facilitate the learners’ analysis and interpretations of their personal and shared experiences during the clinical encounters (39). During the process of experiential learning, the learners are left on their own to work out the steps involved in a specific clinical situation that leads to improved learning and retention in novices than a robust guided protocol (40).
Clinical debrief is a professional discussion platform that integrates the experiences and observations of everyone involved in the exercise into a cohesive argument (41). An effective debrief is a comprehensive and interactive conversation that engages the learners’ decisions, the impact of those decisions, and an outline of their action plans.
A holistic view of the entire process of clinical reasoning is illustrated in Figure 2 that elaborates the gradual engagement of learners in the learning environment while keeping the context-specific and integrated nature of the exercise.
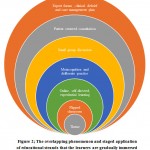 |
Figure 2: The overlapping phenomenon and staged application of educational strands that the learners are gradually immersed during the acquisition of clinical reasoning skills
|
Assessing the clinical reasoning skills
The assessment of CR skills is difficult as these domains are not measurable and academics have to mainly draw inferences from behaviour (42). Due to the context-specific nature of CR, several domains need to be assessed using multiple assessment modalities that can help draw meaningful and valid interpretations. In addition, CR skills should be assessed longitudinally throughout the given module. The taxonomy of teaching strategies for developing CR skills are integrated and linked with feedback and reflection, and its effectiveness can only be materialized if continuous ongoing formative assessment is in place (43). In contrast to the assessment of other domains, the standardization of reliability, feasibility and resource efficacy may appear higher for CR (44).
The modalities that can be employed in assessing CR skills are described below:
Multiple choice question (MCQ) and extended matching question (EMQ)
The MCQs can assess wide content areas and cognitive knowledge across several contexts in a short time (45). The problem solving nature of MCQs can be enhanced by making them contextualised and by inserting clinical scenarios. The EMQs can test reasoning skills by selecting the correct answer from a menu of context-specific clinical situations built around a single theme (46).
Script concordance test (SCT)
“The SCT is based on the principle that the steps in CR process can be assessed and compared to the reasoning ability of a panel of experts” (47). The design of SCT rigorously follows the possible organizational framework of case scripts as elaborated by the domain experts. Initially, an incomplete and vague clinical case script is presented and the learner is asked about a diagnostic hypothesis or clinical impression. Later on, a new information is added in the case script and then the learner is asked as to how this new information would affect his initial clinical judgment.
Long case examination
Long case remains the cornerstone of the majority of clinical examinations where the examinee works-up an allotted (unobserved) case and then presents the same case to the examiner. Though the long case examination is labor-intensive and time-consuming, it provides an opportunity to the examiner to explore the CR process utilized by the examinee. The reliability of long case has been shown to be improved by structuring the examination as in the objective structured clinical examination (48) (49). However, the clinical competence of learners can be improved by understanding their learning styles and adopting the delivery of instructional strategies in concordance with their learning styles (50) (51).
Mini-Clinical Evaluation Exercise (mini-CEX)
The mini-CEX is a component of workplace based assessment, a group of assessment tools that assesses examinee’s performance in real workplace environment (52). The assessor
scores the performance of learner on a standard scoring sheet (global rating) that contains items for the assessment of seven core clinical competencies (medical interviewing, physical exam, medical professionalism, clinical judgment and decision-making, medical counseling, organization/ efficacy and overall clinical competence) (53).. An immediate and contextual feedback is provided by the assessor and the scores of clinical judgment are thought to reflect the level of acquisition of clinical reasoning skills.
Problem-based scenarios
These scenarios challenge several dimensions of a case in a staged fashion, each stage requiring the recording of student reasoning and application of knowledge till the student establishes a management plan.
Portfolios
Portfolios are case records developed and maintained by students illustrating their reflective and narrative writing. These case logs offer authentic evidence of learners’ achievements and can be conveniently used for monitoring and assessing learners’ academic progress and competence (54). “The assessment of portfolios is a powerful approach to assessing a range of curriculum outcomes not easily assessed by other methods and is worthy of inclusion in the assessor’s toolkit” (54).
All the assessment tools described in the preceding section have a pitfall in that all such assessments modes precisely focus on discipline-specific cognitive skills. The process of reasoning in diagnosis is predominantly deductive and the assessment tools rely predominantly on diagnostic reasoning that ignores the ability of learners to critique and reflect about the clinical case. This finding signals the absence of a valid and reliable gold standard tool to assess such a complex skill and demand triangulation of assessment methods to evaluate one or more aspects of the CR process (55).
Study limitations
This systematic review has limitation of being unable to objective assess the effectiveness of CR skills in improving the clinical competence of learners. The teaching and assessment strategies of narrative but conscientious systematic review can be further endorsed by meta-analysis that can determine the effectiveness and impact of CR in health-care practice.
Conclusion and recommendations
The available data envisages the potential role of clinical reasoning in empowering the learners from being collectors and reporters of information to being interpreters of knowledge. Several educational strategies are used during the learners’ acquisition of CR skills; exposure to clinical situations, activation of prior knowledge, development of case scripts, consolidation with experts’ opinions to clinch the most logical diagnosis, encouraging learners to prioritize differential diagnoses, usage of online and face-to-face learning environment, facilitating reflection, metacognition, and deliberate practice. Assessment of clinical reasoning skills should be done throughout the training course in diverse settings and several assessment modes should be used for a holistic evaluation. However, all the suggested assessment modalities primarily focus on diagnostic reasoning that overlooks the student’s ability of critical thinking. Further evidence based research is needed to develop a gold standard assessment tool that can objectively assess all aspects of CR skills.
Conflict of interests
No conflicts declared
References
- Sniderman AD, LaChapelle KJ, Rachon NA, Furberg CD, editors. The necessity for clinical reasoning in the era of evidence-based medicine. Mayo Clinic Proceedings; 2013: Elsevier.
- Linn A, Khaw C, Kildea H, Tonkin A. Clinical reasoning: A guide to improving teaching and practice. Australian family physician. 2012;41(1/2):18.
- Posel N, Mcgee JB, Fleiszer DM. Twelve tips to support the development of clinical reasoning skills using virtual patient cases. Medical teacher. 2015;37(9):813-8.
CrossRef - Custers EJ. Medical education and cognitive continuum theory: an alternative perspective on medical problem solving and clinical reasoning. Academic Medicine. 2013;88(8):1074-80.
CrossRef - Edwards I, Jones M, Carr J, Braunack-Mayer A, Jensen GM. Clinical reasoning strategies in physical therapy. Physical therapy. 2004;84(4):312-30.
- Guraya SY, London N, Guraya SS. Ethics in medical research. Journal of Microscopy and Ultrastructure. 2014;2(3):121-6.
CrossRef - Elstein AS. Thinking about diagnostic thinking: a 30-year perspective. Advances in health sciences education. 2009;14(1):7-18.
CrossRef - Kassirer JP. Teaching clinical reasoning: case-based and coached. Academic Medicine. 2010;85(7):1118-24.
CrossRef - Graber ML. Educational strategies to reduce diagnostic error: can you teach this stuff? Advances in health sciences education. 2009;14(1):63-9.
CrossRef - Durning SJ, Ratcliffe T, Artino Jr AR, van der Vleuten C, Beckman TJ, Holmboe E, et al. How is clinical reasoning developed, maintained, and objectively assessed? Views from expert internists and internal medicine interns. Journal of Continuing Education in the Health Professions. 2013;33(4):215-23.
CrossRef - Charlin B, Boshuizen H, Custers EJ, Feltovich PJ. Scripts and clinical reasoning. Medical education. 2007;41(12):1178-84.
CrossRef - Patel R, Sandars J, Carr S. Clinical diagnostic decision-making in real life contexts: A trans-theoretical approach for teaching: AMEE Guide No. 95. Medical teacher. 2015;37(3):211-27.
CrossRef - Durning S, Artino AR, Pangaro L, van der Vleuten CP, Schuwirth L. Context and clinical reasoning: understanding the perspective of the expert’s voice. Medical education. 2011;45(9):927-38.
CrossRef - Dhaliwal G. Developing teachers of clinical reasoning. The clinical teacher. 2013;10(5):313-7.
CrossRef - Atkinson K, Ajjawi R, Cooling N. Promoting clinical reasoning in general practice trainees: role of the clinical teacher. The clinical teacher. 2011;8(3):176-80.
CrossRef - Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015;4(1):1.
CrossRef - Wolpaw T, Papp KK, Bordage G. Using SNAPPS to facilitate the expression of clinical reasoning and uncertainties: a randomized comparison group trial. Academic Medicine. 2009;84(4):517-24.
CrossRef - Neher JO, Stevens NG. The one-minute preceptor: shaping the teaching conversation. Family medicine kanas city-. 2003;35(6):391-3.
- Audétat M-C, Laurin S, Sanche G, Béïque C, Fon NC, Blais J-G, et al. Clinical reasoning difficulties: A taxonomy for clinical teachers. Medical teacher. 2013;35(3):e984-e9.
CrossRef - Dhaliwal G, Sharpe BA. Twelve tips for presenting a clinical problem solving exercise. Medical teacher. 2009;31(12):1056-9.
CrossRef - Carol-anne EM, Regehr G, Mylopoulos M, MacRae HM. Slowing down when you should: a new model of expert judgment. Academic Medicine. 2007;82(10):S109-S16.
- Ford CL, Yore LD. Toward convergence of critical thinking, metacognition, and reflection: Illustrations from natural and social sciences, teacher education, and classroom practice. Metacognition in science education: Springer; 2012. p. 251-71.
- Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic Medicine. 2004;79(10):S70-S81.
CrossRef - Orrock P, Grace S, Vaughan B, Coutts R. Developing a viva exam to assess clinical reasoning in pre-registration osteopathy students. BMC medical education. 2014;14(1):1.
CrossRef - Maudsley G, Strivens J. Promoting professional knowledge, experiential learning and critical thinking for medical students. Medical education. 2000;34(7):535-44.
CrossRef - Morgan H, McLean K, Chapman C, Fitzgerald J, Yousuf A, Hammoud M. The flipped classroom for medical students. The clinical teacher. 2015;12(3):155-60.
CrossRef - Mayer RE. Applying the science of learning: evidence-based principles for the design of multimedia instruction. American Psychologist. 2008;63(8):760.
CrossRef - Prober CG, Khan S. Medical education reimagined: a call to action. Academic Medicine. 2013;88(10):1407-10.
CrossRef - Tune JD, Sturek M, Basile DP. Flipped classroom model improves graduate student performance in cardiovascular, respiratory, and renal physiology. Advances in physiology education. 2013;37(4):316-20.
CrossRef - Roehl A, Reddy SL, Shannon GJ. The flipped classroom: An opportunity to engage millennial students through active learning. Journal of Family and Consumer Sciences. 2013;105(2):44.
CrossRef - Missildine K, Fountain R, Summers L, Gosselin K. Flipping the classroom to improve student performance and satisfaction. Journal of Nursing Education. 2013.
CrossRef - Harris A, Boyce P, Ajjawi R. Clinical reasoning sessions: back to the patient. The clinical teacher. 2011;8(1):13-6.
CrossRef - Canfield PJ, Whitehead ML, Johnson R, O’Brien CR, Malik R. Case-based clinical reasoning in feline medicine 1: Intuitive and analytical systems. Journal of feline medicine and surgery. 2016;18(1):35-45.
CrossRef - Thistlethwaite JE, Jordan JJ. Patient‐centred consultations: a comparison of student experience and understanding in two clinical environments. Medical education. 1999;33(9):678-85.
CrossRef - Evans B, Coman G, Goss B. Consulting skills training and medical students’ interviewing efficiency. Medical education. 1996;30(2):121-8.
CrossRef - Clack GB. Medical graduates evaluate the effectiveness of their education. Medical education. 1994;28(5):418-31.
CrossRef - Usherwood T. Subjective and behavioural evaluation of the teaching of patient interview skills. Medical education. 1993;27(1):41-7.
CrossRef - McGill I, Weil SW. Continuing the dialogue: new possibilities for experiential learning. Making sense of experiential learning. 1989;249.
- Carr S, Carmody D. Experiential learning in women’s health: medical student reflections. Medical education. 2006;40(8):768-74.
CrossRef - Yardley S, Teunissen PW, Dornan T. Experiential learning: AMEE guide No. 63. Medical teacher. 2012;34(2):e102-e15.
CrossRef - Arora S, Ahmed M, Paige J, Nestel D, Runnacles J, Hull L, et al. Objective structured assessment of debriefing: bringing science to the art of debriefing in surgery. Annals of surgery. 2012;256(6):982-8.
CrossRef - Modi JN, Gupta P, Singh T. Teaching and assessing clinical reasoning skills. Indian pediatrics. 2015;52(9):787-94.
CrossRef - Groves M, Scott I, Alexander H. Assessing clinical reasoning: a method to monitor its development in a PBL curriculum. Medical teacher. 2002;24(5):507-15.
CrossRef - Banning M. Clinical reasoning and its application to nursing: concepts and research studies. Nurse education in practice. 2008;8(3):177-83.
CrossRef - Donnelly C. The Use of Case Based Multiple Choice Questions for Assessing Large Group Teaching: Implications on Student’s Learning. Irish Journal of Academic Practice. 2014;3(1):12.
- Beullens J, Struyf E, Van Damme B. Do extended matching multiple‐choice questions measure clinical reasoning? Medical education. 2005;39(4):410-7.
CrossRef - Lubarsky S, Dory V, Duggan P, Gagnon R, Charlin B. Script concordance testing: From theory to practice: AMEE Guide No. 75. Medical teacher. 2013;35(3):184-93.
CrossRef - Guraya S, Alzobydi A, Salman S. Objective structured clinical examination: Examiners’ bias and recommendations to improve its reliability. J Med Med Sci. 2010;1(7):269-72.
- Shumway J, Harden R. AMEE Guide No. 25: The assessment of learning outcomes for the competent and reflective physician. Medical teacher. 2003;25(6):569-84.
CrossRef - Guraya SY, Forgione A, Gianluca S, Pugliese R. The mapping of preferred resources for surgical education: Perceptions of surgical trainees at the Advanced International Minimally Invasive Surgery Academy (AIMS), Milan, Italy. Journal of Taibah University Medical Sciences. 2015;10(4):396-404.
CrossRef - Guraya SS, Guraya SY, Habib FA, Khoshhal KI. Learning styles of medical students at Taibah University: Trends and implications. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences. 2014;19(12):1155.
CrossRef - Guraya SY. Workplace-based assessment; applications and educational impact. Malaysian Journal of Medical Sciences. 2015;22(6):5-10.
- Norcini JJ, Blank LL, Arnold GK, Kimball HR. The mini-CEX (clinical evaluation exercise): a preliminary investigation. Annals of internal medicine. 1995;123(10):795-9.
CrossRef - Driessen EW, Overeem K, Van Tartwijk J, Van Der Vleuten CP, Muijtjens AM. Validity of portfolio assessment: which qualities determine ratings? Medical education. 2006;40(9):862-6.
CrossRef - Groves M, Dick M-L, McColl G, Bilszta J. Analysing clinical reasoning characteristics using a combined methods approach. BMC medical education. 2013;13(1):144.
CrossRef

This work is licensed under a Creative Commons Attribution 4.0 International License.





