How to Cite | Publication History | PlumX Article Matrix
Features of the Uterine Cavity in Patients with Myoma
Irina Arkadievna Ozerskaya1, Mikhail V. Medvedev1, Natalia Anatolyevna Altynnik1, Yakov Aleksandrovich Lobachev1 and Alexander A. Devitskiy2
1Federal state budgetary educational institution of additional professional education “The Institute of advanced training of Federal medical-biological Agency” Volokolamskoe sh. 91, Moscow, 125371, Russia.
2First Moscow State Medical University named after I. M. Sechenov Malaya Trubetskaya str. 8-2, Moscow, 119991, Russia.
DOI : http://dx.doi.org/10.13005/bbra/2359
ABSTRACT: Was carried out a comparison of the thickness and volume of the endometrium in healthy women and patients with uterine myoma. According to the age composition all groups were similar and consisted of patients of reproductive age and of premenopausal age. Was revealed a significant (p<0.05) excess of the volume of the uterine cavity in both phases of the menstrual cycle in women suffering from uterine fibroids, in comparison with the control group. Among patients with fibroids along with the growth of the volume of the uterus was detected a significant (p<0.05) increase in endometrium, while the thickness of the median complex was not changed.
KEYWORDS: ultrasound; uterine myomas; endometrium
Download this article as:| Copy the following to cite this article: Ozerskaya I. A, Medvedev M. V, Altynnik N. A, Lobachev Y. A, Devitskiy A. A. Features of the Uterine Cavity in Patients with Myoma. Biosci Biotech Res Asia 2016;13(4). |
| Copy the following to cite this URL: Ozerskaya I. A, Medvedev M. V, Altynnik N. A, Lobachev Y. A, Devitskiy A. A. Features of the Uterine Cavity in Patients with Myoma. Biosci Biotech Res Asia 2016;13(4). Available from: https://www.biotech-asia.org/?p=16736 |
Introduction
The problem of ultrasound diagnosis of uterine fibroids is a subject of many scientific papers, and currently it is generally accepted that sonography is a leading instrumental method of identifying the disease. In the scientific literature are discussed the issues of localization, size, structure and blood supply of the myomatous nodes (Demidov, Zykin, 1990; Zykin, Medvedev, 2000; Fedorova, Lipman, 2002; Ozerskaya, 2013; Fascilla, Cramarossa, Cannone, 2016). Data were presented regarding the ultrasonic criteria of the complications of fibroids and principles of differential diagnosis with benign and malignant diseases (Chekalova, Zuev, 2004; Ozerskaya, Ageyeva, 2009; Medvedev, Rud’ko, 2010; Bulanov, 2014; Takeda, Nakamura, 2016). However, it was not given enough attention for the condition of the uterus in patients with fibroids. The purpose of the present study was to change this situation.
Methods
Were examined 72 patients with uterine fibroids in reproductive and premenopausal periods, whose average age was 42 + 7.9 years (ranging from 23 to 56 years). The control group consisted of 73 women with a mean age of 39 + 6.8 years (from 26 to 54 years), with no gynecological pathology. The distribution of patients by age and phases of the menstrual cycle are presented in table 1.
Table 1: The distribution of patients by age and phases of the menstrual cycle
| The phase of the cycle | Uterine myoma | Control group | ||
| n | Age (M+σ) | n | Age (M+σ) | |
| The early proliferative (day 4-9) | 36 | 40.5+8.2 | 22 | 41.1+8.0 |
| Late proliferative (day 10-13) | 15 | 42.7+6.5 | 16 | 39.9+5.6 |
| Secretory | 21 | 42.4+8.0 | 35 | 39.1+6.8 |
Note: the significance of differences between groups of patients and a control group as well as between the phases of the cycle, p>0.05.
Asymptomatic fibroids were noted in 23 women (31.9%). Menstrual irregularities and (or) pain syndrome were observed in 44 (61,1%) patients. Among them, for a hypermenstrual syndrome (hyper–poly–proyomenorea in isolation or in various combinations) were complained of 31 (70,5%) female patient, for the irregular menstruation – 16 (27.5 per cent), for the secondary dysmenorrhea in 9 women (20,5%). Hypomenstrual syndrome was noted in 5 (6,9%) women. The chronic pelvic pain (not related to the menstrual cycle) – in 15 (20,8%). Scrapping of the uterine cavity because of the uterine bleeding and (or) hyperplastic process of the endometrium underwent 11 (15,3%) patients.
Ultrasound examination was carried out on the apparatus Voluson 730 Expert (GE, Austria) by the multifrequency transducers with the transabdominal and transvaginal access in a traditional method. When measuring the volume of the uterus and endometrium was used a software, with the corresponding function of the device with the inherent formula of ovoid: V=АхВхСх0,523, where A, B and C – are the three mutually perpendicular linear dimensions (figure 1, 2). In connection with a high measurement error of the endometrium volume in patients with submucosal location of the node, such patients were not included in the study.
 |
Figure 1: The measurement of the length and anteroposterior size of the uterus and endometrium in the sagittal plane scanning
|
 |
Figure 2: Measurement of the transverse size of the uterus and endometrium while a transverse scanning
|
The obtained results were processed by standard statistical methods. All quantitative data were obeying to a normal distribution, presented as M±s. In those cases, when data did not obey a normal distribution, they were presented as the median (med) and as 5 and 95 percentiles. To identify differences in quantitative traits between the groups we used univariate analysis of variance and bilateral Student t-test. Differences were considered significant at p < 0.05.
The results of the study
At the studying of a control group the volume of the uterine body was in the range of 22.7–72.6 cm3 with an average value of 44.2+13,9 cm3. Any significant differences between phases of the menstrual cycle were not obtained (p>0.05).
The thickness of the endometrium in the early proliferative phase ranged from 2 to 10 mm (4.9+2.3 mm), in the late proliferative phase – from 2 to 11 mm or 6.3+2.6 mm), increasing in the secretory phase from 7 to 15 mm (10,1+2.3 mm). Differences between phases were significant (p<0.05).
The volume of the endometrium in the early proliferative phase ranged from 0.4 to 4.6 cm3 (med 1,7 cm3) and in the late proliferative – from 0.8 to 7.0 CC (med 2,3 cm3) without significant differences in the rate (p>0.05). In the secretory phase of the cycle the endometrial volume increased from 1.7 to 9.1 cm3 (med 4,2 cm3) (p<0,5). Volume changes of endometrial thickness and endometrial volume, depending on the phase of the cycle, are presented in table 2.
Table 2: The volume of the body of the uterus, the thickness and volume of the endometrium in patients of the control group
| The volume of the uterus (M+σ) | The thickness of the endometrium (M+σ) | The volume of the endometrium (med, 5 and 95 percentile) | |
| Early proliferative | 40,3+13,5 | 4,9+2,3 | 1,7 (0,6–4,3) |
| Late proliferative | 42,6+12,7* | 6,4+2,6** | 2,3 (1,0–6,6)* |
| Secretory | 47,1+13,5* | 10,1+2,3** | 4,2 (1,8–7,4)** |
Note: *– reliability of differences of indicators between the cycle phases >0,05; **– reliability of differences of indicators between cycle phases <0,05.
Pathology of the myometrium, endometrium and (or) ovaries of patients of a control group was not revealed.
The volume of the uterus affected by fibroids, ranged from 25,2 to 450,0 cm3, it was met among women in the early proliferative phase (med 87,0 cm3). In the late proliferative and secretory phase fluctuations between the minimum and maximum values of the volume of the uterus were less significant and amounted to 49.5–203,4 cm3 and 42.5–242,4 cm3, respectively (med 102,2 and 98,1 cm3). Any significant differences between the cycle phases were not obtained (p>0.05).
A single myomatous node was detected in 27 (37,5%) women, two nodes – in 10 (13.9%) and multiple in 35 (48.6 percent). Isolated lesions of posterior wall were observed in 20 (27.8 percent) cases, the front – 12 (16,7%), the bottom – 7 (9,7%), the nodes at both walls – 33 (45,8%). The combination of myoma in the body of the uterus and cervical-isthmical region were observed in 8 (11,1%) patients. Interstitial and (or) interstitial-subserous location were identified in 58 (80,6%) cases, centripetally growth – in 8 (11,1%), subserous fibroids on a wide or narrow base – in 7 (9.7 per cent). The minimum average diameter of the tumor was 6 mm, maximum – 55 mm (med 20 mm).
Among patients with myoma the uterine endometrial thickness in the I phase of the cycle ranged from 2 to 14 mm, from 4-th to 9-th day of cycle the median was 5 mm, and from 10-th to 14-th day – 6 mm (p>0.05). In the second phase the endometrial thickness ranged from 2 to 17 mm (mеd 7 mm) (p>0.05). Any significant difference in endometrial volume trough the different phases of the cycle were not obtained. So, in the early proliferative phase the fluctuations were between 0.8 and 12.2 cm3 (mеd of 3.9 cm3), in late – from 1.9 to 9.4 cm3 (mеd of 6.6 cm3) and secretory – between 1.7 and 16.7 cm3 (mеd of 7.9 cm3). The structure and echogenicity of the endometrium in 47 (65,3%) patients was consistent with the phase of the menstrual cycle, while in 19 (26,4%) cases was observed lag of a secretory transformation as in I and the II phases of the cycle, and in 6 (8.3%) was observed hyperechogenic endometrium in the first phase. The basal layer in 38 (27,4%) women was indistinct and uneven.
The volume of the body of the uterus, the thickness and volume of the endometrium in patients with myoma with accuracy rates compared to the control group are presented in table 3.
Table 3: The volume of the body of the uterus, the thickness and volume of the endometrium in patients with hysteromyoma.
| The volume of the uterus
(med, 5 and 95 percentile) |
The thickness of the endometrium
(med, 5 and 95 percentile) |
р between groups | The volume of the endometrium (med, 5 and 95 percentile) | р between groups | |
| Early proliferative | 87,0 (47,5-312,9) | 5 (3-9) | >0,05 | 3,9 (1,1–10,4) | <0,05 |
| Late proliferative | 102,2 (62,8-189,8)* | 6 (3-11)* | >0,05 | 6,6 (2,3–9,3)* | <0,05 |
| Secretory | 98,1 (48,7-204,1)* | 7 (3,5-14,8)* | <0,05 | 7,9 (2,1–16,4)* | <0,05 |
Note: *– reliability of differences of indicators between cycle phases >0,05.
The thicknesses of the endometrium among patients with fibroids did not depend on the volume of the uterus, while the volume of the endometrium in these patients increased with the increasing of a size of the uterus affected by fibroids.
Was made an analysis of the distribution of patients undergoing curettage of the uterus because of the uterine bleeding, depending on the volume of the uterus. It was found that among women with uterine volume of up to 75 cm3 there were no intrauterine interventions on this occasion. Among 17 patients in whom the uterus was from 75 to 100 cm3, 3 patients (17,6%) underwent the curettage of the uterus. In 18 patients with uterine volume from 100 to 150 cm3 an uterine bleeding was observed in 6 (33,5%) cases. Women with uterine volume of more than 150 cm3 were 14 people, among them 2 patients t (14,3%) – underwent dilatation and curettage of the cavity.
Any structural pathology of the ovaries in patients with uterine myoma was not detected.
Discussion
Uterine fibroids are the most common benign tumor of the myometrium, which affects about 20% of women older than 30-35 years (Vikhlyaeva, 2004; Tikhomirov, Lubnin, 2006; Borgfeldt, Andolf, 2000). In younger women fibroids are found much less frequently, and in children and adolescents – it is an exclusive disease (Borgfeldt, Andolf, 2000; Moroni, Vieira, Ferriani, et al., 2015). A. L. Tikhomirov and D. M. Lubnin (2006) noted that in patients at the age of 22-23 years are diagnosed predominantly interstitial-subserous fibroids. In the current study these data are confirmed. Thus, among the 8 women whose age was from 23 to 30 years, subserous and interstitial-subserous site location was noted in 6 cases, and interstitial – only in two.
Asymptomatic fibroids are observed in approximately one third of patients with uterine myoma (Vikhlyaeva, 2004; Ishchenko, Botwin, Leninskiy, 2010). Menstrual cycle for the majority of domestic and foreign researchers is the most frequent clinical symptom.
Hypermenstrual syndrome may be associated not only with submucous location of the node, but also with the violation of the contractile activity of the uterus, dilation of the cavity and, consequently, with an increase in the area of the endometrial rejection (Ishchenko, Botwin, Lenchinskiy, 2010; Savitsky, Savitsky, 2003).
The results of the study showed that in the control group, the thickening of the endometrium is synchronous with an increase of the endometrial volume from the early proliferative to the secretory phase of the menstrual cycle (figure 3).
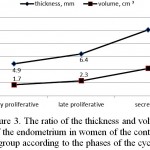 |
Figure 3: The ratio of the thickness and volume of the endometrium in women of the control group according to the phases of the cycle
|
In patients with uterine myoma the endometrial thickness in the I phase did not differ from the values of healthy women of similar age, but beginning from the late proliferative phase the increase in thickness significantly (p<0.05) slows down. At the same time, the volume of the endometrium continues to grow (figure 4).
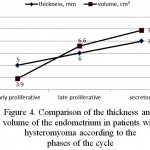 |
Figure 4: Comparison of the thickness and volume of the endometrium in patients with hysteromyoma according to the phases of the cycle
|
When comparing the values of thickness of the endometrium in patients with myoma and control groups was revealed a significant (p<0.05) reduction only in the secretory phase, whereas in phase I the performance is virtually identical (figure 5).
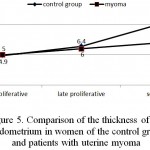 |
Figure 5: Comparison of the thickness of the endometrium in women of the control group and patients with uterine myoma
|
The volume of the endometrium in patients with myoma in both phases of the cycle was almost in 2 times more than in women in the control group (figure 6).
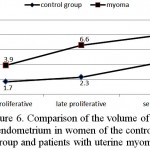 |
Figure 6: Comparison of the volume of the endometrium in women of the control group and patients with uterine myoma
|
In addition, noteworthy is the steady increase in the absence of changes in the thickness of the endometrium as the growth of myoma of the uterus (figure 7).
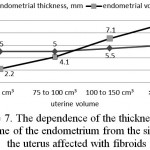 |
Figure 7: The dependence of the thickness and volume of the endometrium from the size of the uterus affected with fibroids
|
Both facts prove the increase of the uterine cavity. In the work of G. A. Savitsky and A. G. Savitsky (2003) is indicated that the area of the endometrium in women with fibroids, consistent with 8-9 weeks of pregnancy increases by more than 1.5 times, consistent with 12 weeks – by more than 3.5 times, and 16 weeks – by more than 5.5 times. However, the visual changes of the thickness of the endometrium with hysteroscopy were not detected (Bacsko G. et al., 1997) (Bacsko, Major, Csiszár, Borsos, 1997).
Among clinicians there is no consensus about the tone of the affected uterine myometrium in the mechanism of uterine bleeding. So, A. I. Ischenko et al. (2010) believe that the trigger of menorrhagia and metrorrhagia is a hypotension of the myometrium, and G. A. Savitsky and A. G. Savitsky (2003) – a hypertension. According to I. S. Sidorova (2003) the presence of simple fibroids is much less likely to cause uterine bleeding than proliferating fibroids. Often a combination of fibroids and endometrial hyperplasia can also be the cause of hyperpolymenorrhea (Tikhomirov, Lubnin, 2006; Sidorova, 2003; Lalonde, 1994; Galen, Isaacson, Lee, 2013). Despite the fact that among the surveyed patients with myoma the hyperplastic processes of the endometrium were absent, the combination of these hormone-dependent diseases does not exclude.
In this study is marked a dependence of the frequency of curettage of the uterine cavity due to bleedings on the uterus volume. So, in the group of patients with the uterus, which volume do not exceed 75 cm3, there were no intrauterine interventions on this occasion. With the increase in the uterus of up to 100 cm3, the curettage was done in 17.6% of women, in the uterus of up to 150 cm3– in 33,5%. It was probably associated with the increased area of desquamation. Among women with uterine volume of more than 150 cm3 a frequency of operative hemostasis was 14.3%, which can be associated with a greater frequency of operative treatment of myoma in the early stages and if patients had such enlarged uterus, reaching in the work in maximum of up to 450 cm3, at the same time the clinical manifestations of the disease were not so significant. In addition, a shown increase in a volume of the endometrium according to the growth of myoma of the and a reducing in the frequency of curettage of the cavity in patients with uterus of more than 150 cm3, confirms polyetiological nature of hypermenstrual syndrome.
Conclusion
According to the conducted research we can draw the following conclusions:
The thickness of the endometrium in patients with uterine myoma in the I phase of the cycle does not differ from the healthy women.
In the second phase of the cycle in patients with uterine fibroids the processes of secretory transformation are slowing. This contributes to the reducing of thickness of the endometrium.
The volume of the endometrium in patients with myoma is more in both phases of the cycle compared with the control group and it increases at the growth of the uterus.
Thus, not only determining the thickness but also the volume of the endometrium allows us better define the condition of the uterine cavity. This method allows to assess endometrial pathology such as diffuse hyperplasia and polyp, and to conduct differential diagnostics between benign and malignant processes.
Reference
- Bacsko, G., Major, T., Csiszár, P., Borsos, A. (1997). Operative hysteroscopy: minimally invasive surgery to control of menorrhagia (vol. 36 (1-4), pp. 7-8). Acta Chirurgica Hungarica. https://www.researchgate.net/publication/ 13822511_Operative_hysteroscopy_minimally_invasive_surgery_to_control_of_menorrhagia
- Borgfeldt, C., Andolf, E. (2000). Transvaginal ultrasonographic findings in the uterus and the endometrium: low prevalence of leiomyoma in a random sample of women age 25-40 years (vol. 79(3), pp. 202-207). Acta Obstetricia et Gynecologica Scandinavica. http://doi/10.1034/j.1600-0412.2000.079003202.x/ full
CrossRef - Fascilla, F.D., Cramarossa, P., Cannone, R. et al. (2016). Ultrasound diagnosis of uterine myomas (vol. 68(3), pp. 297-312). Minerva Ginecologica. http://www.minervamedica.it/en/journals/minerva-ginecologica/article.php?cod=R09Y2016N03A0297
- Galen, D.I., Isaacson, K.B., Lee, B.B. (2013). Does menstrual bleeding decrease after ablation of intramural myomas? A retrospective study (vol. 20(6), pp. 830-835). Journal of Minimally Invasive Gynecology. hppt://doi: 10.1016/j.jmig.2013.05.007.
CrossRef - Lalonde, A. (1994). Evaluation of surgical options in menorrhagia (vol. 101(11), pp. 8-14). British Journal of Obstetric and Gynaecology.
CrossRef - Moroni, R.M., Vieira, C.S., Ferriani, R.A. et al. (2015). Presentation and treatment of uterine leiomyoma in adolescence: a systematic review (vol. 15(4)). BMC Women’s Health.
CrossRef - Takeda, A., Nakamura, H. (2016). Torsion of a Subserosal Myoma Managed by Gasless Laparoendoscopic Single-Site Myomectomy with In-Bag Manual Extraction (pp. 783-1270). Case Reports in Obstetric and Gynecology. http://doi: 10.1155/2016/7831270.
CrossRef - Bulanov, M.N. (2014). Ultrasound gynecology: a course of lectures in two parts. (3rd ed. EXT., part 1). Moscow: Publishing house Vidar-M.
- Vikhlyaeva, E. M. (2004). Guide to the diagnosis and treatment of uterine leiomyoma. Moscow, M: Medpress-inform.
- Demidov, V. N., Zykin, B. I. (1990). Ultrasound diagnosis in gynecology. Moscow, M: Medicine.
- Zykin B. I. Medvedev, M. V. (2000). Doppler ultrasound in gynecology. Moscow, M: Real time.
- Ischenko A. I., Botvin M. A., Lanchinskiy, V. I. (2010). Uterine fibroids: etiology, pathogenesis, diagnostics, treatment. Moscow: Publishing house Vidar-M.
- Medvedev, M. V., Rudko, G. G. (2010). Differential diagnostic ultrasound in gynecology (2nd ed., Rev.). Moscow, M: Real Time.
- Ozerskaya I. A. (2013). Sonography in gynecology. (2nd ed., Rev.), M: Publishing house Vidar-M.
- Ozerskaya I. A., Ageeva, M. I. (2009). Chronic pelvic pain in women of reproductive age. Ultrasound diagnosis. Moscow: Publishing house Vidar-M.
- Savitsky, G. A., Savitsky, A. G. (2003). Uterine fibroids (problems of pathogenesis and pathogenetic therapy). (Ed. 3.). Saint Petersburg, St. Petersburg: ELBI-SPb.
- Sidorova, I. S. (2003). Hysteromyoma (modern issues of etiology, pathogenesis, diagnosis, and treatment). Moscow, M: MIA.
- Tikhomirov A. L., Lubnin D. M. (2006). Myoma of the uterus. Moscow, M: Medical information Agency.
- Fedorova, E. V., Lipman, A. D. (2002). The use of color Doppler mapping and Dopplermetry in gynecology. Moscow: Vidar.
- Chekalova, M. A., Zuev, V. M. (2004). Ultrasound diagnosis in gynecological Oncology. Moscow: Russian doctor.

This work is licensed under a Creative Commons Attribution 4.0 International License.





