How to Cite | Publication History | PlumX Article Matrix
Chronic Headache: The Only Manifestation of Cerebellar Tuberculoma
Diwan Israr Khan* , M Anas, Abiha A Khan and Samreen Khan
, M Anas, Abiha A Khan and Samreen Khan
Ajmal Khan Tibbiya College and hospital, Aligarh Muslim University, Aligarh, India
Corresponding Author Email: israrjnmch@gmail.com
DOI : http://dx.doi.org/10.13005/bbra/2786
ABSTRACT: Despite of availability of highly efficacious treatment for decades, tuberculosis remains a major global health problem in developing countries, like India where tuberculosis is an endemic disease.1 Tuberculous involvement of brain is a rare presentation of extra pulmonary tuberculosis. The infection usually gets access to the brain through hematogenous route. The disease commonly affects children with equal involvement of both sexes and has close association with HIV. The usual manifestation of the disease is fever, unexplained weight loss, nausea, vomiting, headache, seizures, behavioral changes, focal neurological deficit and gait difficulty. Here is a case of cerebellar tuberculoma in an 8 years old male presenting as chronic headache for one and half years.
KEYWORDS: Children; Headache; Tuberculoma; Tuberculosis; ; Endemic Disease; Extra Pulmonary Tuberculosis
Download this article as:| Copy the following to cite this article: Khan D. I, Anas M, Khan A. A, Khan S. Chronic Headache: The Only Manifestation of Cerebellar Tuberculoma. Biosci Biotech Res Asia 2019; 16(4). |
| Copy the following to cite this URL: Khan D. I, Anas M, Khan A. A, Khan S. Chronic Headache: The Only Manifestation of Cerebellar Tuberculoma. Biosci Biotech Res Asia 2019; 16(4). Available from: https://bit.ly/39yU1v8 |
Background
CNS tuberculosis is common in developing countries of tropical areas, often occurs in close association with compromised host’s immunity. The disease has a wide variation in presentation.16 The diagnosis has always been a clinical challenge due to overlapping of symptoms with other diseases.17 The MRI brain has the potential to differentiate the disease from other intracraniallesions.19 The anti-tubercular treatment has always been a mainstay of management with significant outcome.18
Introduction
Tuberculosis is the 9th leading cause of death world wide. Among extra pulmonary tuberculosis, CNS tuberculosis is the most severe form of tuberculosis and accounts approximately 5-10% of all extra pulmonary cases and 1% of all tuberculosis cases.1 CNS tuberculosis primarily menifests as tuberculous meningitis and less commonly as intracranial tuberculoma, tuberculous brain abscess, non-osseous spinal cord tuberculosis, spinal cord tuberculous meningitis, tuberculous encephalopathy, Pott’s spine and Pott’s paraplegia. A tuberculoma is a clinical manifestation of tuberculosis which conglomerates tubercles into a firm lump, and hence imitates malignant tumors in imaging studies .2 The disease may occur either in isolation or less commonly with tubercular meningitis .13 It constitutes 33% of space occupying lesions of brain in developing countries.5 The usual manifestation of the disease is fever, unexplained weight loss, nausea, vomiting, headache, seizures, behavioural changes and focal neurological deficit. Menifestation of any one or two of the above symptoms will hardly lead the physician think about brain tuberculosis. We hereby present a case of a male child who had been presented with chronic headache only, with no other associated symptoms.
Case Report
Irfan, an 8 years old male had been presented to the paediatrics OPD in Ajmal Khan Tibbiya College Hospital, A.M.U. Aligarh, with chief complaint of headache for the last 1.5 years. For the same, his parents consulted various practitioners but the diagnosis was not made. Detailed history revealed that he had no H/O vomiting, weight loss, abnormal movements, focal neurological deficit, and weakness of any body part, cough, change in behavioural and sleep pattern or any other respiratory difficulties. On general examination, the child was vitally stable with BP measuring 100/64 mmHg and a palpable lymph node in left cervical region which was soft and non-tender with size equal to 1.2×1.2cm. The systemic examination revealed that the child was active and alert with no cranial nerves deficit, meningeal or cerebellar signs. Tone and power were normal in all four limbs. The respiratory and cardiac examinations were normal except for a slight decrease in air entry on left side of the chest. The child was then subjected to further work up.The CBC report, fundus and visual acquity test were WNL.Mntx was strongly positive with induration of 25mmx 28mm/72hrs. The X-ray chest revealed consolidation in the left lower lobe of lung with B/L hilar prominence. The FNAC of the cervical lymph node showed reactive lymphadenitis. With the above clues, the MRI brain was done which supported the diagnosis. The findings were suggestive of few irregular hypointense lesions with peri-lesional edema involving right cerebellar hemisphere, cortical grey matter of left parafalcine parieto-occipital lobe and right peri-rolandic parietal lobe (tubercular etiology). With all the above evidences, the diagnosis was inclined to cerebellar tuberculoma. As the treatment protocol, anti-tubercular therapy in the regimen of 2HRZE+10HRE was started along with systemic steroids. The patient responded well to the above treatment. Within 2-3 months, improvement in clinical as well as radiological findings was noted. After that the patient was lost to follow-up.
Discussion
Intracranial tuberculoma is a rare condition accounting 1% of all tubercular cases. The disease is commonly spotted in paediatric age group but involvement of children below 4 years of age is rarely seen. The commonest route of spread is hematogenous from the occult primary focus. The symptoms are usually vague and range from mild persistent headache to acute diplopia or focal neurological deficit.9, 10, 15 The symptoms overlap with other neurological diseases and make the diagnosis difficult. In our case, because of the presence of a non-specific complaint of isolated persistent headache, the diagnosis was delayed. The other risk factors for the disease to occur include, immunosuppressed patients, malnutrition, alcoholism and malignancy.3 When brain tuberculomas are associated with meningitis, the diagnosis is more apparent and would be discovered early. Half of the patients show no clinical signs of involvement of sites other than CNS.7 62% patients with tuberculoma complain about headache.8 The diagnosis is based on imaging with CT/MRI brain. It shows ring enhancing lesion with surrounding edema and is usually single and centralized. But in one-third cases, the lesion may be multiple and peripheral.It may mimic other space occupying lesions and thus needs to be differentiated from malignancy, sarcoidosis, toxoplasmosis and neurocysticercosis.6
 |
Figure 1: Child with positive Tuberculin Skin Test. Click here to view figure |
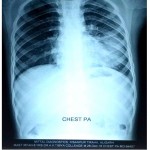 |
Figure 2: Consolidation of Left lower lung field with bilateral dense hila Click here to view figure |
 |
Figure 3: MRI showing few irregular hypo intense lesions with peri-lesional edema involving right cerebellar hemispheres with ventricular dilatation (tubercular etiology) Click here to view figure |
Brain mass biopsy with histopathological evaluation is the gold standard for diagnosis which shows necrotizing granuloma. Tissue biopsy on culture, results in the growth of Mycobacterium tuberculosis.4 Until and unless there are features of raised intracranial tension and peri-lesional edema, the disease should be treated with anti-tubercular drugs. But the duration of therapy is not described. The treatment is modified on the basis of improvement in clinical and radiological findings. Occasionally, development of new lesions or enlargement of the pre-existing lesion may occur during the course of treatment,11 but with adequate therapy, complete resolution of the lesion usually occurs.14 In case of peri-lesional oedema, additional therapy with systemic steroids for a period of 6-8 weeks along with ATT gives promising results. Surgical resection of mass with decompression is done followed by ATT, if there are features of raised ICT.4
Conclusion
In developing countries, tuberculosis has been a huge public health issue with adverse CNScomplications.12 CNS involvement of tuberculosis is rare but most severe, and has a high rate of mortality as well as neurological residual sequelae, despite of the treatment. For this reason, when evaluating common complaints such as headache, especially in subjects with malnutrition, close tubercular contact, immunocompromised and low socio-economic status, a braod differential diagnosis should be considered including brain tuberculosis.4
References
- Practice trend in treating in CNS tuberculosis and outcomes at a tertiary care hospital:A cohort study of 244 cases(Vinay Goyal, Arunmozhimaran Elavarari, Abhishek, Garima Shukla, Madhuri Bihari//www.annalsofin.org/).
- Tuberculoma//en.m.wikipedia.org>wiki
- Cerebral tuberculomas-A clinical challenge(Regina Monteiro, Jose carlos Carneiro,[…], and Raquel Duarte//www.ncbi.nlm.nih.gov/).
- The importance of a complete differential:Case report of a tuberculoma in a patient without pulmonary involvement (Pooja Sethi, Jennifer Treece,[…], and Siddharth Singh//www.ncbi.nlm.nih.gov/ ).
- Brain Tuberculomas: A case report(Maryam Saleh, Ali Asghar Saeedi, and Ali Ali Pooran//www.ncbi.nlm.nih.gov/).
- Tuberculoma of brain- A diagnostic dilemma:Magnetic resonance spectroscopy a new ray of hope (Subhasis Mukherjee, Runa Das, Shabana Begum//www.jacpjournal.org/).
- Multiple Brain Tuberculomas in a 32 years old Woman with chronic headache(Fatehmeh Ahmadi MD, Jalil Feizi MD,Mohammad Sharmardi PhD Candidate//www.ncbi.nlm.nih.gov/).
- Tuberculomas of Brain with or without associated meningitis: A cohort of 28 cases treated with anti-tubercular drugs at a tertiary care centre(Irfan Ahmed Shah, Ravouf Parvaiz Asimi, Yuman Hussain Sarmast www.ijcmr.com>ijcm).
- Tuberculosis (Cliford C. Dacso, in Office Practice of Neurology, Second Edition 2003 sciencedirect.com).
- Tuberculosis of the Central Nervous System (John M. Leonard, in Aminoff’s Neurology and General Medicine Fifth Edition, 2014 www.sciencedirect.com).
- Cerebral tuberculoma (P Dennison G Rajakaruna www.thorax.bmj.com).
- Brain tuberculoma, an unusual cause of stroke in a child with trisomy 21: A case report (Abdelmoneim E.M. Kheir, Salah A. Ibrahim,[…] Farouk A. Hamid www.casereports.biomedcentral.com).
- Central Nervous System Tuberculosis: Pathogenesis and Clinical Aspects(R. Bryan Rock, MichaelOlin,[…], and Phillip K. Peterson// www.ncbi.nim.nih.gov/).
- Central Nervous System Tuberculosis: An Imaging –Focused Review of a Reemerging Disease (Morteza Sanei Taheri, Mohammad Ali Karimi, Hamidreza Haghighatkhah, Ramin Pourghorban, Mohammad Samadian, and Hosein Delavar Kasmaei www.hindawi.com).
- Clinical Syndromes and Cardinal Features of Infectious Diseases: Approach to Diagnosis and Initial Management (Douglas Swanson, Christopher J. Harrison, in Principles and Practice of Paediatric Infectious Diseases Fourth Edition, 2012 www.sciencedirect.com).
- Intracisternal tuberculoma: a refractory type of tuberculoma indicating surgical intervention (Fanfan Chen, Lei Chen, […] Hongbin Ju, BMC Neurology www.bmcneurol.biomedcentral.com).
- Disseminated cerebral and spinal tuberculomas: rare cause of triparesis ( Rajesh Verma and Aveg Bhandari //www.ncbi.nlm.nih.gov/).
- Central Nervous System Tuberculoma Complicated with Spinal Arachnoiditis in Immunocompetent Patient (A.A. Ayu Suryapraba, Ni Made Susilawathi, and I wayan Niryana //www.ncbi.nlm.nih.gov/).
- Intracranial tuberculoma and recent advances in magnetic resonance imaging ( Ahmad A Moussa, Mohamed E. Mahmoud and Hosam A. Yousef www.//ejns.springeropen.com)

This work is licensed under a Creative Commons Attribution 4.0 International License.





