How to Cite | Publication History | PlumX Article Matrix
Nasser Alqahtani1* , Wala Alzahrani1
, Wala Alzahrani1 , Mona Abosamrah1
, Mona Abosamrah1 , Waseem Fatima1
, Waseem Fatima1 , Ansh Garwal2
, Ansh Garwal2 , Amer Alanazi3
, Amer Alanazi3
1Clinical Nutrition Department, Faculty of Applied Medical Sciences, Northern Border University, Arar, Saudi Arabia.
2Faculty of Medicine, Northern Border University, Arar, Saudi Arabia,
3Northern Medical Tower, Directorate of Health Affairs in Northern Border Region, Ministry of Health, Arar, Saudi Arabia.
Corresponding Author E-mail: nalqahtaniphd@gmail.com
DOI : http://dx.doi.org/10.13005/bbra/2975
ABSTRACT: Background: Vitamin D deficiency is currently recognized as a global epidemic and has been linked to many diseases. According to recent studies in Saudi Arabia showed a high prevalence of Saudi population having vitamin D deficiency. Objectives: The objective of this project was to find out how common vitamin D grade is and to look at the relationship between body fat proportion and vitamin D status among female university students. Methods: University female students were the subject of a cross-sectional study. After obtaining their permission, sample of 300 students were selected to participate. Weight, height and waist circumference were taken. Body composition were analyzed by using bioelectrical impedance analysis (BIA). Bloodspot testing was used to determine 25 hydroxyvitamin D (25(OH) D) level. Results: this research found significant relationship between vitamin D deficiency and the body fat percentage. Overweight and obese people have lower vitamin D levels than slimmer people. The relationship between the two variables is medium strong and inverse meaning that students with high proportion of body fat have decreased levels of vitamin D and vice versa. This finding is supported by the linear regression model between the two variables that reveals that if all factors affecting vitamin D status are held constant, the percentage body fat explains 28.2% of the variability in the vitamin D status. Conclusion: In conclusion, there is a statistically significant connotation between body fat and vitamin D status amongst female students. Further investigation is in need to tackle this health issue.
KEYWORDS: Body Fat; BMI; Overweight; Obesity; Vitamin D status
Download this article as:| Copy the following to cite this article: Alqahtani N, Alzahrani W, Abosamrah M, Fatima W, Garwal A, Alanazi A. Association between Vitamin D status and body composition: a cross-sectional study among University Female Students. Biosci Biotech Res Asia 2022;19(1). |
| Copy the following to cite this URL: Alqahtani N, Alzahrani W, Abosamrah M, Fatima W, Garwal A, Alanazi A. Association between Vitamin D status and body composition: a cross-sectional study among University Female Students. Biosci Biotech Res Asia 2022;19(1). Available from: https://bit.ly/3qJ1diw |
Introduction
Vitamin D insufficiency is now recognized as a worldwide problem 1;2 with approximately over 1 billion people globally have vitamin D deficiency 3; 4. It has been linked with many non-musculoskeletal chronic diseases such as cardiovascular diseases 5;6and diabetes mellitus 7; 8.
A major cause of vitamin D deficiency is insufficient exposure to sunlight, wearing of covering clothes and using sunscreen 9 and it depends on the activity of the enzymes responsible for its final hydroxylation 10. Some food items naturally contain vitamin D, and fortified food with vitamin D are often insufficient 11;12.
According to a new study, 83.6% of Saudi population having vitamin D deficiency. Comparing to males, females are severely vitamin D deficient 13. Even the Kingdom of Saudi Arabia (KSA) is considered a sunny country all over, except in winter, but they found certain factors as dress styles and regions were associated with the low of vitamin D (13). Florez et al. (2007) 14 reported that low levels of vitamin D concentrations were among the obese participants. Accordingly, the high frequency of low vitamin D status was associated of overweight and obesity 15. Together, the high prevalence of obesity and low vitamin D status, have been linked to many chronic illnesses like cancer, type2 diabetes, heart diseases 16.
As a result, more study is being conducted to better understand the relationship between vitamin D status and obesity 15. Saudi Arabia and other countries in the Middle East have high prevalence of vitamin D deficiency status and obesity 16; 17. Even though, studies in the Middle East investigating the association between vitamin D status and obesity are limited 18; 19.
According to Gannage et al. (2010)20, 25 (OH) D exposed was in reversely associated by means of Body mass index (BMI) (p < 0.01) and waist circumference (p < 0.01) amongst 381 Lebanese University students.
Nonetheless, Sadiya et al. (2014)19 disclosed that the incidence of vitamin D < 50 nmol/L was 83.2% amongst obese 309 diabetic adults in United Arab Emirate.
Research objectives
The purpose of this project is to investigate the low occurrence of vitamin D status among female university students’ in KSA.
To investigate the relationship between percentage of body fat and vitamin D status.
Literature Review
According to Davis and Dwyer (2007)21, vitamin D is a critical controller of bone breakdown which plays a vital role in adipogenesis and helps to prevent number of sicknesses such as osteoporosis, cancer, diabetes, and immunological disorders. Furthermore, Kremer et al. (2009)22 noted that deficiency of vitamin D is regarded as an epidemic problem due to its association with diminished bone mineral density, an amplified fracture risk, and obesity in adults. Obesity and being overweight are serious public health issues. In 2014, the WHO estimated that 39 percent of individuals were overweight, and 13 percent were obese 23.
Al Nozha et al. (2005)24 stated that the prevalence of overweight and obesity in Saudi Arabia was 36.9% (females 31.8%) and 35.5% (females 44%) respectively.
Vitamin D deficiency can occur mainly because of inadequate exposure to sunlight. Also, the activation of this enzyme depends on the action of the enzymes (25- hydroxylase and 1α- hydroxylase) which are responsible for its final hydroxylation10. Moreover, Moreira and Hamadah (2010)12 thought that vitamin D exists naturally in few foods and the content of this vitamin in the fortified foods is often inadequate and this only account for about 30% of vitamin D. Therefore, the rest of vitamin D is obtained through skin exposure to U.V. radiation which is responsible for the activation of this vitamin into 7- dehydrocholesterol leading to formation of pre-vitamin D3.
Albaik and her colleges (2016)25 found that, compare to normal weight participants, obese cases have been known to have lower vitamin D levels. They investigated the association between serum vitamin D status and BMI among obese women in Saudi Arabia and reported that vitamin D deficiency were common among women in Jeddah, KSA, and that this prevalence is increasing with obesity.
According to Foss YJ. (2009)26, vitamin D deficiency can cause of obesity, and that obesity may be corrected by boosting vitamin D status.
Obesity, on the other hand, is a risk aspect for hypovitaminosis D27, because obese people often have less exposure to sun light because of their limited mobility and they tend to be less physically active, as well as the possible trapping of vitamin D by the adipocytes. Obesity
can contribute to poor vitamin D grade due to the storage of this vitamin in body fat compartments, lowering its bioavailability, and the need for vitamin D to create stronger bones to sustain their increased weight, in addition to clothing preferences.28
Adipogenesis can be repressed by 1,25 dihydroxyvitamin D(29). There is link between the status of vitamin D and body fat, A strong inverse relationship between weight, body mass and vitamin D levels. That s found in young women with decreased vitamin D levels were much heavier and had more body mass compared to women with normal vitamin D levels22.
The vitamin D contributes to body mass maintenance because it tends to lower leptin concentrations 30. The vitamin D status dependence on BMI was studied by Lagunova and her colleagues in 2009 and they concluded that BMI negatively correlated with both serum 25(OH)D3 and 1,25(OH)2D3 31. Also, it was been found that in animal models, body adipose cells can accumulate 10-12% as a supplemented amount of vitamin D 32.
As a result of the above research, it is possible to conclude that obesity is partially, a direct outcome of vitamin D deficiency and may affect in vitamin D deficiency. Furthermore, it is worth noting that vitamin D deficiency can lead to a variety of disorders such as osteoporosis, cancer, diabetes, and rheumatoid arthritis (33), and that excess body fat is strongly connected to an increased risk of diabetes and cancer (34). Consequently, vitamin D deficiency could play a part in the expansion of these diverse clinical diseases, whichever directly or indirectly.
Hypothesis
Our goals are to investigate the relationship anthropometric parameters and status of vitamin D, as well as the relationship between body fat proportion and vitamin D position among university female students in Saudi Arabia.
As a result, we expected that patients with a high total % body fat would have lower serum vitamin D levels.
Research Methodology (Material & Methods)
This is a cross-sectional study was carried out among female students at Northern Border University (NBU) in Arar. After describing the purpose of the study, 300 female students were volunteer to take part in this study
Each participant sign a written informed consent form to participate in the study, which was authorized by the Research Ethics Committee at NBU Faculty of Medicine.
Students having history of renal/hepatic disease, malabsorption, gestation, lactation, a family history of rickets, or who are using anti-convulsant or vitamin D supplements will be disqualified.
Anthropometric assessment
Following an overnight fasting, study participants were asked to the nutrition laboratory for anthropometric collection including height, WC, weight, and body composition.
To measure height to the bordering 0.1 cm, the subsequent procedure was used: no wearing of shoes, heels, while head in contact with the horizontally oriented stadiometer’s ruler.
An un-stretchable tailor’s tape measure was wrapped around the plain abdomen precisely above the hip bone but corresponding to the floor to determine WC.
The InBody720 bioelectrical impedance analyzer (BIA) has been used to determine weight and body composition (Biospace, Seoul, Korea). BIA assesses bodily water before estimating fat and fat free mass. The BIA machine was calibrated before use. After cleaning hands and feet using electrolyte wipes, participants has been requested to stand on the machine barefooted and without any metal/jewelry. BMI is computed as follows: Weight (kg)/ Height (m2). BMI of 18.5 kg/m2 was considered underweight, standard weight of 18.5–24.9 kg/m2, while overweight at 25–29.9 kg/m2, and finally obese at 30 kg/m2 or above.
Vitamin D (25 (OH) D) was measured using vitamin D bloodspot testing
Research Design
Collected data were analyzed using the social sciences statistical tool SPSS.
Chi-square test data was used to assess cluster differences for categorical variables.
P value of < 0.05 was used as statistically significant.
The Saudi Ministry of Health discovered a great prevalence of deprived vitamin D status in adult females and males in Saudi Arabia.
Vitamin D insufficiency was thought to be common among female students at NBU.
The significance of this study stems from the fact that it will compare vitamin D status and percent body fat among female students at Northern Border University.
There has been little or no investigation about the relationship between body fat % and vitamin D status amongst university female students in Arar city.
Results
Table 1: Statistics
| Statistics | |||
| S.No | vitamin D | fat % | age |
| Valid | 65 | 65 | 65 |
| Missing | 0 | 0 | 0 |
| Mean | 24.743 | 25.846 | 22.08 |
| Median | 21.000 | 25.000 | 22.00 |
| Std. Deviation | 9.9709 | 10.1041 | 1.190 |
| Skewness | .785 | .186 | -.841 |
| Std. Error of Skewness | .297 | .297 | .297 |
| Kurtosis | -.532 | -1.527 | -.314 |
| Std. Error of Kurtosis | .586 | .586 | .586 |
| Minimum | 9.9 | 13.0 | 19 |
| Maximum | 45.0 | 45.0 | 24 |
Table 1 above shows the descriptive statistics of vitamin D, fat % and age. The means and median are important measures of central tendency that can be used to determine whether the data follows a normal distribution. From the above table, it is clear that the three variables follow a fairly normal distribution due to the closeness between the values of the mean and median. Fairly normal distribution of the variables is also shown by the values of skewness and kurtosis which are not very far from zero.
Table 2
| Correlations | ||||
| vitamin D | fat % | age | ||
| vitamin D | Pearson Correlation | 1 | -.531** | 0.205 |
| Sig. (2-tailed) | 0.000 | 0.102 | ||
| fat % | Pearson Correlation | -.531** | 1 | -.293* |
| Sig. (2-tailed) | 0.000 | 0.018 | ||
| Age | Pearson Correlation | 0.205 | -.293* | 1 |
| Sig. (2-tailed) | 0.102 | 0.018 | ||
| N | 65 | 65 | 65 | |
Table 2: The correlation coefficients between the variables are shown. The strength of the association between two continuous variables is measured by correlation. The correlation coefficient value goes from -1 to +1 and measures the strength and direction of the link. From the table above, there is a medium strong and inverse relationship between vitamin D and fat %. This means that as fat % increases, vitamin D decreases. As a result of this link between body fat and vitamin D levels, overweight and obese people have lower vitamin D levels than slimmer people. It is crucial to remember, however, that correlation does not indicate causation, which means that being obese does not always and always result in low vitamin D levels.
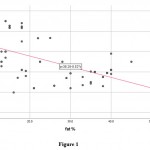 |
Figure 1 |
Figure 1 above is a scatter plot showing the relationship between vitamin D and fat %. A scatter plot is actually a visual representation of correlation and from the scatter plot above, it is clear that there is a negative / inverse relationship between the two variables. The red line is referred to as a line of best fit and it is a linear fit on the scatter plot. The equation of the line above is y = -0.52x + 38.28 which can be interpreted as follows: –
Vitamin D = -0.52*fat % + 38.28. Vitamin D is the dependent or response variable, fat % is the independent or predictor variable, -0.52 is the coefficient of the predictor variable while the value 38.28 is known as the constant.
The negative value of the coefficient of the predictor reveals the inverse relationship between vitamin D and fat %.
Table 3
| Model Summaryb | ||||
| Model | R | R Square | Adjusted R Square | Std. Error of the Estimate |
| 1 | .531a | 0.282 | 0.270 | 8.5165 |
| a. Predictors: (Constant), fat % | ||||
| b. Dependent Variable: vitamin D | ||||
Table 3 above shows the basic statistics after performing a linear regression procedure. R is the coefficient of correlation covered extensively earlier. R square also known as the coefficient of determination is an important measure of goodness of fit of the regression model and it is abbreviated by R2. The R2 value is 0.282 and what this means is that 28.2% of the variability in vitamin D levels is explained by fat % holding other factors constant.
Table 4
| ANOVAa | ||||||
| Model | Sum of Squares | df | Mean Square | F | Sig. | |
| 1 | Regression | 1793.412 | 1 | 1793.412 | 24.727 | .000b |
| Residual | 4569.387 | 63 | 72.530 | |||
| Total | 6362.799 | 64 | ||||
Table 4 is the Analysis of Variance (ANOVA) table and what it basically does in the context of regression is to breakdown the sum of squares, the degrees of freedom, the computed F-statistic, and the p-value. This table is very crucial because it used to determine whether to reject or fail to reject the null hypothesis. The null and alternative hypotheses of linear regression are shown below: –
Null hypothesis, H0: There is no statistically significant linear regression between vitamin D and fat % (β1 = 0)
Alternative hypothesis, H1: There is a statistically significant linear regression between vitamin D and fat % (β1 ≠ 0)
From table 4 above, the p-value is 0.000 which is less than 0.05 and this leads us to reject the null hypothesis and conclude that there is a statistically significant regression between vitamin D and fat %.
Table 5
| Coefficientsa | ||||||
| Model | Unstandardized Coefficients | Standardized Coefficients | t | Sig. | ||
| B | Std. Error | Beta | ||||
| 1 | (Constant) | 38.284 | 2.921 | 13.107 | 0.000 | |
| fat % | -0.524 | 0.105 | -0.531 | -4.973 | 0.000 | |
Table 5 above contains the coefficients of regression and in essence the equation of the regression equation. The equation of the linear regression model can be written as: –
Vitamin D = -0.524*fat % + 38.284
The regression equation above brings out two vital things;
A unit change in fat % leads to a decrease in vitamin D by 0.524 units.
When fat % is 0, the value of vitamin D is 38.28
The t-statistic is an important statistic for each regression coefficient and it is computed by dividing the regression coefficients by the standard error of the coefficients.
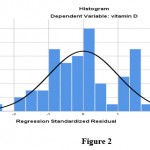 |
Figure 2 |
After a regression analysis, it is important to conduct regression diagnostics to ensure that the regression model does not violate linear regression assumptions. One of the crucial assumptions is that the residuals follow a normal distribution. The residuals or error terms are obtained by getting the difference between the observed and expected values of the dependent variable. From figure 2 above, the histogram shows a fairly normal distribution of the residuals.
 |
Figure 3 |
Figure 3 above shows a standard P-P plot of the residuals.
A P-P normal plot is a visual check on the normality of the distribution of the error terms around the middle of the line of best fit. The normal P-P plot above shows that the points at the middle are close to the line of best fit which means that the normality assumption has not been violated.
Discussion
The above results show that there is a significant relationship between vitamin D deficiency and the body fat %. The three variables in the data set, vitamin D, fat % and age follow a fairly normal distribution which is demonstrated by the closeness between the values of the mean and median. The fairly normal distribution of the variables is also shown by the values of skewness and kurtosis which are not very far from zero.
There exists a medium strong and inverse connection between vitamin D and fat %. This means that as fat % increases, vitamin D decreases. Therefore, according to this relationship between body fat and vitamin D levels, overweight and obese people have lower levels of vitamin D than slimmer people. Nonetheless, it is important to note that this correlation does not imply causality meaning that being obese does not necessarily and automatically lead to low vitamin D levels.
The coefficient of determination (R2) of the regression model is 0.282 and what this means is that 28.2% of the variability in vitamin D levels is explained by fat % holding other factors constant.
The null and alternative hypotheses of linear regression are shown below: –
Null hypothesis, H0: There exists no statistically significant linear regression between vitamin D and fat % (β1 = 0)
Alternative hypothesis, H1: There exists a statistically significant linear regression between vitamin D and fat % (β1 ≠ 0)
From the linear regression results, the p-value is 0.000 which is less than 0.05. Hence we reject the null hypothesis and established that there is a significant regression between vitamin D and fat %.
The equation of the linear regression model is as follows: –
Vitamin D = -0.524*fat % + 38.284
From the regression equation we deduced that:-
A unit change in fat % leads to a decrease in vitamin D by 0.524 units.
When fat % is 0, the value of vitamin D is 38.28
The histogram of the residuals produced as part of post-estimation diagnostic tests shows that the residuals follow a normal distribution and therefore the assumption of normality is satisfied. The normal P-P plot also showed that the normality assumption has not been violated by the regression model between vitamin D and fat percentage.
It is important to mention that vitamin D has strong effectiveness on the epigenome and more than thousand genes inside body cells by activating the VDR. It has been found that the more of gene variants like cholesterol and vitamin D metabolism, the greater the risk of developing vitamin D deficiency.
Conclusion
In conclusion, there is a statistically significant relation between body-fat percentage and vitamin D status amongst female students at NBU in KSA. The relationship between the two variables is medium strong and inverse meaning that students with high proportion of body fat have decreased levels of vitamin D and vice versa. This finding is supported by the linear regression model between the two variables that reveals that if all factors affecting vitamin D status are held constant, the percentage body fat explains 28.2% of the variability in the vitamin D status. These findings corroborate previous studies that have found a link between obesity and low vitamin D levels. Therefore, it is imperative for health officials to generate policies towards reducing the number of overweight and obesity. Further research in order to explore additional factors that affect the vitamin D grade and determine whether there is a causal link between these factors and vitamin D status.
Acknowledgment
This project was supported by Research Deanship, Northern Border University. Researchers would like to thank Faculty staff, Mukhlid Alanazi, Muneef Aalanazi and Zyad Alanazi for their assistance in this research.
Conflict of Interests
The authors have no conflicts of interest to declare.
Funding Sources
This research was funded by Deanship of Research, Northern Border University, Arar. Grant number 1113-AMS-2018-3-9-F.
References
- Batieha, A., Khader, Y., Jaddou, H., Hyassat, D., Batieha, Z., Khateeb, M., Belbisi, A. & Ajlouni, K. 2011, “Vitamin D Status in Jordan: Dress Style and Gender Discrepancies”, Annals of Nutrition and Metabolism, vol. 58, no. 1, pp. 10-18. https://doi.org/10.1159/000323097
CrossRef - Binkley, N., MD, Ramamurthy, R., MD & Krueger, D., BS 2010, “Low Vitamin D Status: Definition, Prevalence, Consequences, and Correction”, Endocrinology and Metabolism Clinics, vol. 39, no. 2, pp. 287-301. https://doi.org/10.1016/j.ecl.2010.02.008
CrossRef - Adams, J.S. & Hewison, M. 2010, “Update in vitamin D”, journal Clinical Endocrinal and Metabolism.no.95,pp.471–478 https://academic.oup.com/jcem/article/95/2/471/2596417
CrossRef - Holick, M.F. & Chen, T.C. 2008, “Vitamin D deficiency: a worldwide problem with health consequences”, The American journal of clinical nutrition, vol. 87, no. 4, pp. 1080S-1086S. https://academic.oup.com/ajcn/article/87/4/1080S/4633477?referringRepId=115375
CrossRef - Reid, I.R. & Bolland, M.J. 2012, “Role of vitamin D deficiency in cardiovascular disease”, Heart (British Cardiac Society), vol. 98, no. 8, pp. 609-614. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.883.5247&rep=rep1&type=pdf
CrossRef - Ford, J.A., MacLennan, G.S., Avenell, A., Bolland, M., Grey, A., Witham, M., RECORD Trial Group & for the RECORD Trial Group 2014, “Cardiovascular disease and vitamin D supplementation: trial analysis, systematic review, and meta-analysis”, The American journal of clinical nutrition, vol. 100, no. 3, pp. 746-755. https://academic.oup.com/ajcn/article/100/3/746/4576427
CrossRef - Mitri, Joanna, MD, MS & Pittas, Anastassios G., MD, MS 2014, “Vitamin D and Diabetes”, Endocrinology and Metabolism Clinics, vol. 43, no. 1, pp. 205-232 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3942667/
CrossRef - Mitri, J., Muraru, M.D. & Pittas, A.G. 2011, “Vitamin D and type 2 diabetes: a systematic review”, European Journal of Clinical Nutrition, vol. 65, no. 9, pp. 1005- 1015.https://www.nature.com/articles/ejcn2011118
CrossRef - Bouillon, R., Carmeliet, G., Verlinden, L., van Etten E, Vertuyf A, Luderer HF, Liebeb L, Demay M. 2008, Vitamin D and Human Health: Lessons from Vitamin D Receptor Null Mice. Endocrine Reviews. 29:726–776. https://academic.oup.com/edrv/article/29/6/726/2355027
CrossRef - Engelsen, O. 2010, “The relationship between ultraviolet radiation exposure and vitamin D status”, Nutrients, vol. 2, no. 5, pp. 482-495 https://www.mdpi.com/2072-6643/2/5/482/pdf
CrossRef - Zhang, R. & Naughton, D.P. 2010, “Vitamin D in health and disease: current perspectives”, Nutrition journal, vol. 9, no. 1, pp. 65-65. https://scindeks.ceon.rs/article.aspx?artid=0365-44781901116C&lang=en
CrossRef - Moreira, T. S. & Hamadeh, M. J. 2010, “The Role of Vitamin D Deficiency in the Pathgenesis of Type 2 Diabetes Mellitus. e-SPEN”, The European e- Journal of Clinical Nutrition and Metabolism. 85, no. 5, pp. 155- 165. DOI: 10.2337/db08-0593
CrossRef - Nabi, G., Hobani, Y. & Sarwat, M. 2015, “High prevalence of vitamin D deficiency and cancer in Saudi Arabian populations: Can we hypothesize a link?”, Medical Hypotheses, vol. 85, no. 2, pp. 117-119. https://www.academia.edu/download/39822449/med_hypo.pdf
CrossRef - Florez, H., Martinez, R., Chacra, W., Strickman-Stein, N. & Levis, S. 2007, “Outdoor exercise reduces the risk of hypovitaminosis D in the obese”, Journal of Steroid Biochemistry and Molecular Biology, vol. 103, no. 3-5, pp. 679-681. https://www.mdpi.com/2072-6643/5/3/949/pdf
CrossRef - Vanlint, S. 2013, “Vitamin D and obesity”, Nutrients, vol. 5, no. 3, pp. 949-956 https://www.mdpi.com/2072-6643/5/3/949/pdf
CrossRef - Hoteit, M., Al-Shaar, L., Yazbeck, C., Bou Sleiman, M., Ghalayini, T. & El-Hajj Fuleihan, G. 2014, “Hypovitaminosis D in a sunny country: Time trends, predictors, and implications for practice guidelines”, Metabolism, vol. 63, no. 7, pp. 968-978. https://www.aub.edu.lb/fm/CaMOP/publications/Hypovitaminosis-D-in-a-sunny-country-Time-trends.pdf
CrossRef - Fuleihan G. 2009,”Vitamin D deficiency in the Middle East and its health consequences”. In: Holick MF vitamin D: physiology, molecular biology, and clinical applications. 2nd edition. New Jersey: Humana Press. https://research.vumc.nl/ws/files/187350/237115.pdf
- Sadiya, A., Ahmed, S.M., Skaria, S. & Abusnana, S. 2014, “Vitamin D status and its relationship with metabolic markers in persons with obesity and type 2 diabetes in the UAE: a cross-sectional study”, Journal of diabetes research, vol. 2014, pp. 869307-7. https://www.hindawi.com/journals/jdr/2014/869307/
CrossRef - Gannage-Yared, M.H., Chedid, R., Khalife, S., Azzi, E., Zoghbi, F., & Halaby, G. 2009,” Vitamin D in relation to metabolic risk factors, insulin sensitivity and adiponectin in a young middle-eastern population”, Europe journal Endocrinology, vol. 160, no.6 pp. 965–71. https://eje.bioscientifica.com/view/journals/eje/160/6/965.xml
CrossRef - Davis, C.D. & Dwyer, J.T. 2007, “The “sunshine vitamin”: benefits beyond bone?”, Journal of the National Cancer Institute, vol. 99, no. 21, pp. 1563-1565 https://www.direct-ms.org/wp-content/uploads/2018/01/Cancer-Vit-D-editorial-JNCI-07.pdf
CrossRef - Kremer, R., Campbell, P., Reinhardt, T. & Vicente Gilsanz .2009, “Vitamin D Status and Its Relationship to Body Fat, Final Height, and Peak Bone Mass in Young Women”, Journal of Clinical Endocrinology Metabolism, 94, pp. 67–73.
CrossRef - – WHO: World Health Organization. Obesity and Overweight. Available at: http://www.who.int/mediacentre/factsheets/fs311/en/. #Last Editorial Review (January, 2015).
- Al-Nozha, M.M., Al-Mazrou, Y.Y., Al-Maatouq, M.A., Arafah, M.R., Khalil, M.Z., Khan, N.B., Al-Marzouki, K., Abdullah, M.A., Al-Khadra, A.H., Al-Harthi, S.S., Al-Shahid, M.S., Al-Mobeireek, A. & Nouh, M.S. 2005, “Obesity in Saudi Arabia”, Saudi medical journal, 26, no. 5, pp. 824. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.920.4569&rep=rep1&type=pdf
- Albaik, M., Khan, J., Ardawi, M., & Moselhy, S. 2016, “Correlation between Serum Vitamin D Status and Body Mass Index in Obese Women”, International Journal of Life Sciences Research, Vol. no. 4, pp. 277-235. https://www.researchgate.net/profile/Mai-Albaik/publication/290428516_Correlation_between_Serum_Vitamin_D_Status_and_Body_Mass_Index_in_Obese_Women/links/579fbb2c08aece1c72156883/Correlation-between-Serum-Vitamin-D-Status-and-Body-Mass-Index-in-Obese-Women.pdf
- Foss, Y.J. 2008;2009;, “Vitamin D deficiency is the cause of common obesity”, Medical Hypotheses, vol. 72, no. 3, pp. 314-321. https://www.sciencedirect.com/science/article/pii/S0306987708005288
CrossRef - Larrroude, M., Moggia, M., Díaz, R., Pérez Sainz, M., Macías, G. & Man, Z. 2009, “Prevalence of deficit of vitamin D in patients with overweight and obesity”, Bone, vol. 45, no. 6, pp. S149-S149. https://www.infona.pl/resource/bwmeta1.element.elsevier-a4a9c874-1e2c-3153-bfcf-da5f6350cadd
CrossRef - Renzaho, A.M.N., Ph.D., Halliday, Jennifer A., B.H.Sci. (Hons) & Nowson, C., Ph.D 2011, “Vitamin D, obesity, and obesity-related chronic disease among ethnic minorities: A systematic review”, Nutrition, vol. 27, no. 9, pp. 868-879. http://www.glnbi.org/documenti/5f49a53b49b6f1817d185f5ea0357819.pdf
CrossRef - Kong, J. & Li, Y.C.2006, “Molecular mechanism of 1, 25-dihydroxyvitamin D3 inhibition of adipogenesis in 3T3-L1 cells”,American Journal of Physiology- Endocrinology and Metabolism, vol. 290 , pp. 916 – 924. https://journals.physiology.org/doi/full/10.1152/ajpendo.00410.2005
CrossRef - Menendez, C., Lage, M., Peino, R., Baldelli, R., Concheiro, P., Diéguez, C. & Casanueva, F.F. 2001, “Retinoic acid and vitamin D(3) powerfully inhibit in vitro leptin secretion by human adipose tissue”, The Journal of endocrinology, vol. 170, no. 2, pp. 425-431. https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.335.5754&rep=rep1&type=pdf
CrossRef - Lagunova, Z., Porojnicu, A., Lindberg, F., Hexeberg, S. & Moan, J. 2009, “The dependency of vitamin D status on body mass index, gender, age and season”, Obesity and metabolism, vol. , no. 4, pp. 52. https://ar.iiarjournals.org/content/anticanres/29/9/3713.full.pdf
CrossRef - Rosenstreich, S.J, Rich, C. &Volwiler, W. 1971, “Deposition in and release of vitamin D3 from body fat: evidence for a storage site in the rat”, Journal of Clinical Investigation, vol. 50, pp. 679-687. https://www.jci.org/articles/view/106538/files/pdf
CrossRef - Zmuda, J.M., Cauley, J.A. & Ferrell, R.E. 2000, “Molecular epidemiology of vitamin D receptor gene variants“, Epidemiolgy Reviw, vol. 9, no. 22, pp. 203–217 http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.327.7222&rep=rep1&type=pdf
CrossRef - Holick, M.F. 2004, “Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis”, American Journal of Clinical Nutrition, vol. 79, pp.362–371. https://academic.oup.com/ajcn/article/79/3/362/4690120?ijkey=d1349735a1bf5e1899458369092bf421bd19cee6&keytype2=tf_ipsecsh
CrossRef

This work is licensed under a Creative Commons Attribution 4.0 International License.





