How to Cite | Publication History | PlumX Article Matrix
E. F. Osagiede1,2 , N. S. Awunor3*
, N. S. Awunor3* , E. T. Osagiede4
, E. T. Osagiede4 and S. O. Abah5
and S. O. Abah5
1Department of Community Medicine, Irrua Specialist Teaching Hospital, Irrua, Nigeria.
2Department of Community Medicine, Niger Delta University Teaching Hospital, Okolobiri, Nigeria.
3Department of Community Medicine, Delta State University Abraka, Nigeria.
4Accident and Emergency Unit, Irrua Specialist Teaching Hospital, Irrua, Nigeria.
5Department of Community Health and Primary Health Care, Ambrose Alli University Ekpoma, Nigeria.
Corresponding Author E-mail: awunorca@delsu.edu.ng
DOI : http://dx.doi.org/10.13005/bbra/2985
ABSTRACT:
Hepatitis B and C viral infections are amongst the most critical occupation-related infections in the hospital workplace. This study assesses the determinants of uptake and completion of hepatitis B vaccine amongst health care personnel (HCP) in a tertiary health facility in South-South, Nigeria. This study employs a descriptive cross-sectional study design, and data were collected using a quantitative method. Pre-tested, semi-structured interviewer-administered questionnaires were administered to 280 HCP. The IBM SPSS version 21.0 was used for data analysis. About half of HCP had received the first dose of the hepatitis B vaccine, with less than half of that number completing the third dose. It is significantly higher amongst the core healthcare professionals than the non-healthcare professionals. There is a high drop-out rate in the hepatitis B vaccination process which was more amongst the non-clinical group than the clinical. The short duration of work (1-5 years) is a significant predictor of initiation of the vaccination process, while good knowledge of hepatitis B and C viruses was a strong predictor for complete uptake. This study reveals a fair uptake of the first dose of hepatitis B vaccine amongst HCP with a high drop-out rate and a concomitant low completion of the vaccine course amongst respondents. Priority should be given to ensure planned programmes that will help enhance optimal uptake of hepatitis B vaccine amongst HCP.
KEYWORDS: Hepatitis B vaccination; Healthcare Personnel; Predictors, Uptake; Vaccine Knowledge
Download this article as:| Copy the following to cite this article: Osagiede E. F, Awunor N. S, Osagiede E. T, Abah S. O. Predictors of Uptake and Completion of Hepatitis B Vaccine amongst Health Care Personnel in a Rural Teaching Hospital in South-South Nigeria. Biosci Biotech Res Asia 2022;19(1). |
| Copy the following to cite this URL: Osagiede E. F, Awunor N. S, Osagiede E. T, Abah S. O. Predictors of Uptake and Completion of Hepatitis B Vaccine amongst Health Care Personnel in a Rural Teaching Hospital in South-South Nigeria. Biosci Biotech Res Asia 2022;19(1). Available from: https://bit.ly/3rs4Aec |
Introduction
Hepatitis B vaccine is the first anti-cancer vaccine that has an exceptional record of safety and effectiveness. The vaccine is 95% effective in preventing children and adults from developing chronic infections.1 At present, vaccination against hepatitis B virus (HBV), which was introduced in 1992, is the surest way to avoid acquiring hepatitis B infection as a healthcare setting occupational disease and in other settings.2 The hepatitis B vaccine is now one of the most widely used vaccines in the world. Since 1982, over one billion doses of the hepatitis B vaccine have been used worldwide. The most currently available forms of hepatitis B vaccines are produced via recombinant DNA technology. The vaccines are typically given in a three-dose series at day zero, one month later, and six months later.3 A booster dose(s) is not usually recommended for persons who have completed the three-dose vaccination schedule.1 The magnitude of HBV infection has reduced in several countries due to the universal vaccination programmes, which started in the nineties. The infection is, however, still responsible for a vast socio-economic burden in several developing countries like Nigeria.4
Generally, HBV infection is highly endemic in Nigeria based on studies undertaken in blood donors, pregnant women, and HIV-infected patients. These studies reveal an HBsAg carrier rate of 9% to 39%.5,6 An investigation states that in 2010 Edo State in South-South Nigeria had a low immunization coverage, with only 13% of children aged between 12 and 23 months receiving the recommended course of immunization.7 The same survey reports that 27% of the children of the same age group never received any form of immunization in their lifetime, including the hepatitis B vaccine.7 Consequently, the risk of occupational exposure to HBV amongst healthcare personnel in Nigeria remains high.8 Despite this high rate of exposure and its high HBV prevalence, there is conversely a low corresponding vaccination coverage amongst healthcare personnel in Nigeria and some other African countries.8 Although a few studies have been conducted on selected health care personnel (HCP) in Nigeria, the findings also reveal low rates of HBV vaccination coverage of 20%–50%.9–11
In a cross-sectional study carried out amongst healthcare workers at the University of Nigeria Teaching Hospital, Enugu, only 22.4% of healthcare workers had received the hepatitis B vaccine.9 The drop-out rate amongst Nigerian HCP seems to be similar to findings from other African countries, but this is not without variation from one region to another. In both studies carried out in Lagos and Enugu, Nigeria, of the 54% and 22.4% who received hepatitis B vaccine, only 16.4% and 3.7% received a full dose, respectively.9,12 Other fairly higher coverage rates reveal single dosage uptake rates as 64.5% and 70.2% and a completion rate of 36.2% and 59.4%, respectively.8,13
Vaccination against HBV in West African nations (Nigeria inclusive) is lower than in many other countries in other regions of sub-Sahara Africa.14 Also, in other parts of Africa, the coverage rate of hepatitis B vaccination is generally low. A cross-sectional study carried in Burkina Faso amongst 452 health care workers (HCWs) and South Africa reveals that only 10.9% and 19.9% respectively had complete hepatitis B vaccination with a high drop-out rate recorded in both studies.15,16 Findings from a meta-analysis of previous studies published beyond the year 2000 in the sub-Saharan African subregion, including 41 studies, shows that although the awareness of HBV and hepatitis B vaccination amongst HCP were relatively high, vaccination rates were lower, with 4.6–64.4% of the respondents who got “ever vaccinated” completing the course.17
On the contrary, HBV infection is less endemic in the developed world. In sustaining this low transmission rate, prevention strategies through vaccination are sustained at the present optimal level. For the high-risk group like the HCP, vaccination coverage rates are far higher in developed countries than in the world’s developing countries. For instance, a survey of 425 hospitals in America comprising of 6,116 HCP such as nurses, phlebotomists, nurses’ aide/other patient care staff, physicians, maintenance/home-keeping staff, and administrative staff between 2002 and 2003, reveals that the coverage rate of hepatitis B vaccination was as high as 75%.18 In this multi-center study, the coverage rates for physicians and nurses were 81.6% and 80.9%, respectively.18 Similarly, in a descriptive study involving 430 surgeons from three Iranian universities and one national annual surgical society, a similar result is found with a vaccination coverage rate of 76%.19
A probe into the possible cause of this low uptake of hepatitis B vaccination in Nigeria shows that it may not be strictly hepatitis B vaccine knowledge-related. The level of awareness of the hepatitis B vaccine is significantly high amongst HCP in Nigeria.8,20–22 Ironically, such a high level of awareness has not translated to good practices amongst the HCP in Nigeria.20 Findings reveal that it was only in studies carried out amongst HCWs of Obafemi Awolowo University Teaching Hospital Complex (OAUTHC) Ile-Ife, in South-West Nigeria, where an increase was recorded from 54% to 65% completing hepatitis B vaccination in a 15year interval.10,23 The researcher attributes the increase in good practice to the occasional hepatitis B vaccination programme in the healthcare facility.20 Also, reports from other centres: Kesieme, in a multi-centre descriptive study of 228 theatre operating personnel of four University Teaching Hospitals, one each in South-South, North-Eastern, South-Western, and South-Eastern geopolitical zones of Nigeria, reports an awareness level of 87% amongst these HCWs but only 27% corresponding vaccination coverage rate.21 In another descriptive study of HCP involving 346 clinical medical students in North Central Nigeria, only 48% completed their hepatitis B vaccination, whereas their awareness level of these respondents was as high as 92%.22 Most of the surveys relating to the uptake of the hepatitis B vaccine have been on the knowledge of hepatitis B vaccine. Unfortunately, there has been no commensurate uptake.
Few other studies have established possible predictors of hepatitis B vaccination uptake and completion beyond respondents’ knowledge of the vaccine. Findings from North Central Nigeria reveal that the poor uptake was due to a lack of opportunity.22 Others attribute the poor uptake to non-availability of the vaccine,8 poor motivation, lack of access to vaccines, cost implications, and risk perception.24 From the literature search, no probe has been done on the general knowledge of HBV and HCV as it may affect the uptake and competition of the hepatitis B vaccine. Good knowledge of these diseases regarding their morbidities, transmission, and other possible prevention methods could be predictors of the hepatitis B vaccine uptake and completion of vaccination by healthcare personnel.
This study, therefore, explores, amongst other things, the HCP knowledge of HBV and hepatitis C virus (HCV), other possible predictors of the uptake and completion of hepatitis B vaccination amongst HCP in a rural teaching hospital in South-South Nigeria.
Materials and Methods
The study was conducted in Irrua Specialist Teaching Hospital (ISTH), Irrua, Edo State, South-South, Nigeria.7 The hospital is one of the two public teaching hospitals in a rural location in South-South, Nigeria.25 Descriptive cross-sectional study design was conducted between February and March 2018 amongst 280 consenting HCP of the health facility. The selection of participants for the study was carried out through a multistage sampling technique. This included stratified random sampling used to select the different categories or subgroups of HCP and systematic random sampling for selecting the actual study participants in each of the subgroups.
The institution serving as a teaching hospital has the following HCP. Viz: Clinical medical students of Ambrose Alli University, midwifery students from St. Camillus Uromi, and post-diploma (basic) nursing students in peri-operatives and theatre nursing undergoing their various postings in the relevant departments and units of the hospital. The core clinical categories of HCP in the hospital are doctors, nurses, laboratory scientists, scientific officers, pharmacists and pharmacy technicians, health attendants, and porters. The non-clinical categories of HCP include administrative officers, confidential secretaries, account and audit staff, divers, engineers, horticulturists, caterers, security personnel, and medical records staff. Using stratified random sampling, the HCP selected for this study were doctors, nurses, laboratory scientists, scientific officers, pharmacists and pharmacy technicians, health attendants, porters, administrative officers, confidential secretaries, account and audit staff. There were 389 doctors, 624 nurses, 84 laboratory scientists, 24 scientific officers, 110 health attendants, 119 porters, and 295 non-clinical health care personnel (246 administrative staff and 49 account/audit departments) in the hospital. This gave rise to 1684 HCP in all the selected subgroups in the hospital.26
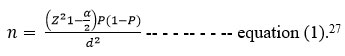
The proportion of HCP in a previous study who had hepatitis B vaccination (uptake rate, P) was 22.4%9. The proportion of the respondents who did not take hepatitis B vaccination among the HCP (1-P) was 77.6%. The standard normal deviate, Z 1-α/2 at 95% confidence interval is 1.96 at two-tailed. The alpha error d is the margin of error allowed for the study, which measures the desired precision/degree of accuracy or deviation, usually at 5%.
Computing for the minimum sample size (n) using the formula given as
Where, p = 22.4% = 0.224 and 1-p = 77.6% = 0.776; d = 5% = 0.05; and z = 1.96.
By substitution into equation (1),
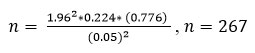
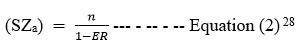
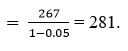
Assuming the completeness rate in interviewers’ filling the questionnaire is 95% [error rate is 5% which is 0.05], the adjusted sample size with the error factor was determined with as sample size
Where ER = error rate.
The adjusted required sample size (SZa) is
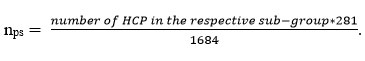
The number of participants selected from each stratum to achieve the desired sample size of 281 was done through a proportionate allocation.
The proportion of participants drawn from each stratum was obtained from the formula as given as = (total number of HCP in a subgroup * adjusted sample size)/total number of HCP in all the subgroups.
The proportion of participants per stratum (nps) is given as
nps = (NHCPsg * SZm)/TNHCP – – – – – – – – – Equation (3)
where;
nps = Proportion of participants per stratum,
NHCPsg = Number of health care personnel (HCP) in a subgroup (stratum),
SZm = Sample size
TNHCP = total number of HCP in all the subgroups
This gave rise to the following numbers of HCP as follows: Doctors – 65, nurses – 104, laboratory scientists and personnel – 14, pharmacists and pharmacy technicians – 6, scientific officers – 4, porters – 20, health attendants – 18, the administrative and secretarial staff – 41, and account and audit staff – 8. After calculating the number of HCP allocated for each stratum, the final participants were identified and recruited through a systematic random sampling technique.29 The list of all nurses, porters, and health attendants was obtained from the director of nursing services. All doctors and laboratory scientists were obtained from the director of clinical services, while the non-clinical staff list was obtained from the hospital registry.
The systematic random sampling technique was carried out as follows. Sampling fraction obtained using the formula, total number of HCWs in the selected subgroups divided by the number allocated by proportionate sampling for the same subgroup of HCWs.
The sampling fraction (Sf) is given as
Sf = NHCPsg / nps — – – – – – – – Equation (4)
where;
NHCPsg = Number of HCP in a subgroup (stratum), and
nps = Proportion of participants per stratum,
By substitution, for example (in the doctors’ subgroup), the sampling fraction for the doctors was obtained as 389/65 = 5.98, approximately 6. Similarly, a sampling fraction of 6 was obtained for all other subgroups of HCP using the same formula. Using the sampling fraction, every 6th HCP in each subgroup was selected from the sampling frame (subgroup total) in the list of the HCP in the given subgroup till the minimum allocated number was selected. The first HCP in each subgroup was selected by balloting between the first to sixth eligible participant on the list. After that, every 6th consenting HCP was picked for the study. The study instrument was a pre-tested, semi-structured, interviewer-administered questionnaire employed to assess the respondents’ sociodemographic characteristics, knowledge of HBV and HCV, the uptake, and completion of hepatitis B vaccination.
The score of knowledge of hepatitis B and C viral infections was based on 38 questions. Each correct answer was scored one, and incorrect answer(s) scored zero (0). The scores obtained were classified thus based on the distribution of the data set.30 It was converted to percentages and graded as poor for less than the mid-mark (<50%). Scores of 50% to 65% were fair, while those greater than 65 % were good. Uptake of hepatitis B vaccine was asked with a “Yes or No” question. The response of a “Yes” to obtain the hepatitis B vaccine was followed with the question of “Number of doses taken.” The number of hepatitis B vaccine doses taken was used to ascertain the completion of the three doses of hepatitis B vaccination. A question on the anatomical site was asked to ascertain further whether the respondent took the vaccine or not. Reasons for not completing the doses were ascertained from those who reported not to have completed the three doses of the hepatitis B vaccine. The vaccination drop-out rate was calculated by dividing the difference in the number of those who took at least a single dose (HB1) and a total of those who took at least three doses (HB3) by the total number of respondents who had at least a single dose (HB1). Subsequently, the results are expressed in percentage.
The drop-out rate (DOR) = [(HB1-HB3)/HB1]*100 – – – – – – – Equation (5)
here;
HB1 = The number of participants who took at least a single (1) dose.
HB3 = The number of participants who took at least three (3) doses.
Variables were measured as nominal, ordinal, and numerical. Frequencies and percentages were derived from the categorical variables. The level of significance – alpha (α) was set at 5%. All p- values were two-tailed and considered as statistically significant if < 0.05. Non-Parametric statistical analysis and the mean (standard deviation) of the univariates data were determined and represented in tables. The bivariate data were analyzed using the Chi-square test (or Fisher’s exact test, where appropriate). In contrast, the multivariate data were analyzed using regression analysis to determine the hepatitis B vaccine uptake predictors.
Ethical approval for the study was obtained from the Health Research and Ethical Committee (HREC) of Irrua Specialist Teaching Hospital, Irrua, Edo State, Nigeria. The purposes and procedures of the research were explained to the respondents. Written informed consent was obtained from them individually. Confidentiality was assured and maintained throughout the study. All forms of personal identifications were avoided during the study. The study’s benefits were explained to the study population that the relevant bodies could utilize the findings from this study to improve their occupational health safety and services.
Results
Two hundred and eighty-one interviewer-administered questionnaires were administered in this survey; two hundred and eighty (280) were utterly administered, given a <1% error rate of administering the questionnaire. The questionnaire was used in this study to determine the HCP knowledge of HBV and HCV. The possible predictors of the uptake and completion of hepatitis B vaccination amongst HCP were also investigated. The results are presented in sections.
Table 1: Sociodemographic Characteristics of Respondents (N=280)
| Variable | Frequency | Percent |
| Age (years) | ||
| 20-29 | 40 | 14.3 |
| 30-39 | 112 | 40.0 |
| 40-49 | 82 | 29.3 |
| 50-59 | 44 | 15.7 |
| 60-69 | 2 | 0.7 |
| Mean ± SD | 34.90 (±9.46) years | |
| Sex | ||
| Male | 104 | 37.1 |
| Female | 176 | 62.9 |
| Job Category | ||
| Nurses | 104 | 37.1 |
| Medical doctors | 65 | 23.2 |
| Administrative and Account officers | 49 | 17.5 |
| Porters | 20 | 7.1 |
| Health attendants | 18 | 6.4 |
| Laboratory scientists/technologists | 14 | 5.0 |
| Pharmacists | 6 | 2.1 |
| Scientific officers | 4 | 1.4 |
| Work Type | ||
| Clinical Related | 231 | 82.5 |
| Non-clinical related | 49 | 17.5 |
| Duration of Work (years) | ||
| <1 | 15 | 5.4 |
| 1-5 | 82 | 29.3 |
| 6-10 | 103 | 36.8 |
| 11-15 | 18 | 6.4 |
| 16-35 | 62 | 22.1 |
| Mean ± SD | 9.64 (±8.26) years |
The mean (and SD) age of the participants is 34.9 (±9.46) years, with 112(40.0%) of them belonging to the age group of 30-39years. Nurses are 104(37.1%), accounting and administrative staff 49(17.5%), health attendants 18 (6.4%), laboratory scientists/technologists 14 (5%), doctors 65(23.2%), while pharmacists, porters, and scientific officers are 6 (2.1%), 20 (7.1%) and 4 (1.4%) respectively. The clinically related work types are 231 (82.5%) while 49 (17.5%) are not (Table 1).31
Uptake and completion of hepatitis B Vaccination
Table 2: Uptake of Hepatitis B Vaccine amongst Healthcare Personnel
| Variable | Frequency | Percent | |
|
S/N |
Hepatitis B vaccine uptake | ||
| A. | A. No single dose (N = 280) | 144 | 51.4 |
| B. | B. At least a dose (N = 280) | 136 | 48.6 |
| B.1 | B.1 Partial vaccination (n=136) | 75 | 55.1 |
| B.2 | B.2 Complete vaccination (n=136) | 61* | 44.9 |
| B.2.1 | B.2.1 Had booster dose(s) (n=61) | 20 | 32.8 |
*Two (3.3%) of the 61 participants who completed their vaccination for hepatitis B reported having had their anti-HBV titre checked.
Slightly more than half (51.4%) of the respondents did not take any dose of the hepatitis B vaccine. Of the 136(48.6%) respondents who took at least a dose of the hepatitis B vaccine, about 45% of them completed their three doses, while only about one-third [20(32.8%)] obtained a booster dose. This survey’s average hepatitis B vaccine drop-out rate was (136-61)/136 = 55.1%. (Table 2)
Table 3: Respondents’ Work Characteristics and Uptake of Hepatitis B Vaccine (N=280).
| Variables | Uptake of hepatitis B vaccine | ||||
| None (%) | Partial (%) | Complete (%) | χ2 | p-value | |
| Work Type | |||||
| Clinical | 112(48.5) | 61(26.4) | 58(25.1) | 8.98 | 0.010* |
| Non-clinical | 32(65.3) | 14(28.6) | 3(6.1) | ||
| Categories of HCP | |||||
| Administrative and account officers | 32(65.3) | 14(28.6) | 3(6.1) | †94.15 | <0.001* |
| Health attendants | 16(88.9) | 2(11.1) | 0(0.0) | ||
| Laboratory Scientists and technologists | 4(28.6) | 6(42.9) | 4(28.6) | ||
| Medical doctors | 15(23.1) | 17(26.2) | 33(50.8) | ||
| Nurses | 53(51.0) | 32(30.8) | 19(18.3) | ||
| Pharmacists | 2(33.3) | 4(66.7) | 0(0.0) | ||
| Porters | 20(100) | 0(0.0) | 0(0.0) | ||
| Scientific officers | 2(50.0) | 0(0.0) | 2(50.0) | ||
| Duration of Work (years) | |||||
| <1 | 6(40.0) | 5(33.3) | 4(26.7) | †21.23 | 0.007* |
| 1-5 | 32(39.0) | 27(32.9) | 23(28.0) | ||
| 6-10 | 69(67.0) | 15(14.6) | 19(18.4) | ||
| 11-15 | 10(55.6) | 5(27.8) | 3(16.7) | ||
| 16-35 | 27(43.5) | 23(37.1) | 12(19.4) | ||
*Statistically significant, † Fisher’s exact test.
There is a statistically significant relationship between uptake of hepatitis B vaccine and work type amongst respondents. About one-quarter (25.1%) of the clinical-related HCP had an uptake of complete doses of hepatitis B vaccine compared to less than one-tenth of the non-clinical HCP. There is also a statistically significant relationship between respondents’ uptake of hepatitis B vaccine job categories. About one-half (50.8%) of the medical doctors had complete doses of hepatitis B vaccine compared to zero proportion recorded amongst the pharmacists, porters, and health attendants for complete doses of hepatitis B vaccination uptake. (Table 3)
Table 4: Knowledge of HBV/ HCV and Uptake of Hepatitis B Vaccine by Respondents (N=280)
| Variables | Uptake of hepatitis B vaccine | ||||
| None (%) | Partial (%) | Complete (%) | χ2 | p-value | |
| Knowledge of HBV and HCV | |||||
| Good | 52(39.1) | 34(25.6) | 47(35.3) | 48.66 | <0.001* |
| Fair | 22(39.3) | 23(41.1) | 11(19.6) | ||
| Poor | 70(76.9) | 18(19.8) | 3(3.3) | ||
*Statistically significant, † Fisher’s exact test.
There is a demonstrable statistically significant relationship between knowledge of HBV/HCV and uptake of hepatitis B vaccine with good knowledge of HBV/HCV associated with more (35%) uptake, and poor knowledge tends to be associated with low (3.3%) uptake. (Table 4)
Table 5: Respondents’ Selected Characteristics and their Practice of Completing Doses (Full Uptake) of Hepatitis B Vaccine
| Variable | Uptake of three doses of Hepatitis B vaccine | χ2 | p-value | |
| n1 = 75 | n2 = 61 | |||
| No (%) | Yes (%) | |||
| Duration of Practice (years) (n = 136) | ||||
| <1 | 4(44.4) | 5(55.6) | 4.00 | 0.404 |
| 1-5 | 27(54.0) | 23(46.0) | ||
| 6-10 | 16(45.7) | 19(54.3) | ||
| 11-15 | 5(71.4) | 2(28.6) | ||
| 16-35 | 23(65.7) | 12(34.3) | ||
| Work Type (n = 136) | ||||
| Clinical Related | 60(50.8) | 58(49.2) | †6.66 | 0.010* |
| Non-clinical Related | 15(83.3) | 3(16.7) | ||
| Job Category (n = 136) | ||||
| Administrative and account Officers | 15(83.3) | 3(16.7) | 25.63 | <0.001* |
| Medical doctors | 16(32.0) | 34(68.0) | ||
| Nurses | 32(64.0) | 16(36.0) | ||
| Laboratory scientists | 6(60.0) | 4(40) | ||
| Scientific Officers | 0(0.0) | 2(100.0) | ||
| Pharmacists | 4(100.0) | 0(0.0) | ||
| Health attendants | 4(100.0) | 0(0.0) | ||
*Statistically significant † Fisher’s exact test.
There is a statistically significant association between workgroup and full uptake (completing three doses) of the hepatitis B vaccine, with the clinically related workgroup being associated with more (49.2%) uptake, and non-clinical related tends to be associated with low (16.7%) uptake. On the job categorization, there is also a statistically significant relationship between job categories and uptake of complete doses of the hepatitis B vaccine with being a scientific officer 100%, medical doctor or laboratory scientists associated with good uptake, followed by being a nurse while being a pharmacist or a health attendant tends to be associated with no uptake of the third dose of hepatitis B vaccination. (Table 5)
Table 6: Reasons for and against the uptake of Hepatitis B Vaccine amongst Healthcare Personnel
| Variable | Frequency | Percent |
| Motivating reasons for uptake | (n =136) | |
| Personal decision | 60 | 44.1 |
| Health education on HBV | 43 | 31.6 |
| Experience at work | 13 | 9.6 |
| Hospital policy | 10 | 7.4 |
| After screening for HBV | 9 | 6.6 |
| Staff orientation | 1 | 0.7 |
| Reasons why the Vaccine was not Received | (n = 144) | |
| Not aware I had to be vaccinated | 37 | 25.7 |
| Vaccine not available when wanted to get vaccinated | 37 | 25.7 |
| No time | 30 | 20.8 |
| Never saw it as important | 23 | 16.0 |
| Not free | 10 | 6.9 |
| Side Effect | 5 | 3.5 |
| Others* | 2 | 1.4 |
| Reasons for not completing vaccine doses | (n =75) | |
| Forgot | 30 | 36.0 |
| Vaccine not available | 22 | 29.3 |
| The next dose is not yet due | 13 | 17.3 |
| Not told to come back for next dose | 7 | 9.3 |
| Too busy at work | 3 | 4.0 |
| Workers industrial action | 1 | 1.3 |
*Doubt efficacy of vaccine [1(0.7%)], Pregnancy [1(0.7%)].
Sixty (44.1%) gave personal decisions as their motivating reasons for obtaining the hepatitis B vaccine. About one-third (31.6%) of the respondents who obtained the hepatitis B vaccine were motivated by health education. Only 1(0.7%) of the respondents got their motivation for the hepatitis B vaccine from the staff orientation they received.
Thirty-seven (25.7%) did not receive the hepatitis B vaccine because they were not aware they had to be vaccinated for the hepatitis B vaccine. The same proportion (25.7%) said the vaccine was unavailable when they wanted to get vaccinated. One (0.7%) each gave pregnancy and doubt of the vaccine’s efficacy as their reason for not receiving the vaccine.
Of those that started the vaccination process that did not complete the three doses, 27(36%) said they forgot they had to come for the next dose of the vaccine, 22(29.3%) said the vaccine was not available, and 7(9.3%) said they were not told to come back. Three (4%) said they were too busy at work. One (1.3%) gave strike (withdrawal of services during industrial disputes) as the reason for not completing their scheduled vaccination. However, thirteen (17.3%) were awaiting their next dose of the hepatitis B vaccine during this survey. (Table 6)
Table 7: Select Characteristics, Hepatitis B Vaccination Status, and Vaccine Drop-out Rate Amongst Respondents
|
Variable |
Hepatitis B vaccination status, n (%) |
χ2 |
p-value
|
Vaccination
drop-out rate (%) |
|
| Partial Complete | |||||
| Knowledge of HBV & HCV infections (n = 136) | (1-2 doses)
n=75 |
(3 doses)
n=61 |
|||
| Good | 33(40.7) | 48(59.3) | 18.29 | <0.001* | 40.7 |
| Fair | 23(69.7) | 10(30.3) | 69.7 | ||
| Poor | 19(86.4) | 3(13.6) | 86.4 | ||
| Duration of Practice (years) (n = 136) | |||||
| <1 | 4(44.4) | 5(55.6) | 4.00 | 0.404 | 44.4 |
| 1-5 | 27(54.0) | 23(46.0) | 54.0 | ||
| 6-10 | 16(45.7) | 19(54.3) | 45.7 | ||
| 11-15 | 5(71.4) | 2(28.6) | 71.4 | ||
| 16-35 | 23(65.7) | 12(34.3) | 65.7 | ||
| Work type (n = 136) | |||||
| Clinical related | 60(50.8) | 58(49.2) | 6.66† | 0.010* | 50.8 |
| Non-clinical related | 15(83.3) | 3(16.7) | 83.3 | ||
| Job Category (n = 136) | |||||
| Administrative and Account Officers | 15(83.3) | 3(16.7) | 25.63 | <0.001* | 83.3 |
| Medical doctors | 16(32.0) | 34(68.0) | 32.0 | ||
| Nurses | 32(64.0) | 16(36.0) | 66.6 | ||
| Laboratory scientists | 6(60.0) | 4(40) | 60.0 | ||
*Statistically significant, † Fisher’s exact test
Respondents’ knowledge of HBV/HCV has a statistically significant relationship with completing the three doses of HB vaccination with an increased drop-out rate with poor knowledge. There is an increase in the drop-out rate in the non-clinically related workgroup than the clinically related without a statistically significant relationship. There is a statistically significant relationship between doctors, nurses, or other clinical-related job categories. Being a doctor tends to be associated with less drop-out rate for HB vaccination, and being in other clinically related groups other than a doctor or a nurse is associated with a higher drop-out rate (Table 7).
Predictors of uptake and completion of hepatitis B Vaccination
Table 8: Predictors of Commencement (Initiating the 1st Dose) of Hepatitis B Vaccine (Binary Multivariate Logistic Regression Model).
| Predictors | β-Coefficient | Odds ratio | 95% Confidence interval | p-value |
| Knowledge of HBV and HCV | ||||
| Poor | Reference | |||
| Fair | 0.627 | 1.872 | (0.837 – 4.188) | 0.127 |
| Good | 0.551 | 1.735 | (0.916 – 3.287) | 0.091 |
| Duration of Practice (years) | ||||
| 6-10 | Reference | |||
| <1 | 1.202 | 3.327 | (0.968 – 11.442) | 0.056 |
| 1-5 | 0.997 | 2.711 | (1.402 – 5.244) | 0.003* |
| 11-15 | 0.206 | 1.229 | (0.408 – 3.696) | 0.714 |
| 16-35 | 1.033 | 2.811 | (1.363 – 5.794) | 0.005* |
| Work Type | ||||
| Non – clinical related | Reference | |||
| Clinical related | -0.566 | 0.568 | (0.243 – 1.325) | 0.190 |
*Statistically significant.
Significantly associated with the uptake of the hepatitis B vaccine with reference to 6-10 years duration was the duration of practice at 1-5 years (p = 0.003) and 16-35 years (p = 0.005), respectively. Respondent’s knowledge of HBV/HCV nor their work type was not associated with the uptake of hepatitis B vaccine (Table 8).
Table 9: Predictors of Uptake Complete (Three) Doses of Hepatitis B Vaccine (Binary Multivariate Logistic Regression Model)
| Predictors | β-Coefficient | Odds ratio | 95% Confidence interval | p-value |
| Knowledge of HBV and HCV | ||||
| Poor | Reference | |||
| Fair | 1.772 | 5.881 | (0.896 – 38.606) | 0.065 |
| Good | 3.043 | 20.978 | (3.061 – 143.744) | 0.002* |
| Duration of Practice (years) | ||||
| 6-10 | Reference | |||
| <1 | -0.559 | 0.572 | (0.109 – 2.998) | 0.509 |
| 1-5 | -0.274 | 0.760 | (0.275 – 2.103 | 0.597 |
| 11-15 | -1.275 | 0.279 | (0.036 – 2.152) | 0.221 |
| 16-35 | -0.990 | 0.372 | (0.109 – 1.262) | 0.113 |
| Work Type | ||||
| Non – clinical related | Reference | |||
| Clinical related | -0.219 | 0.803 | (0.122 – 5.306) | 0.820 |
*Statistically significant.
The data shows that having a good knowledge of HBV/HCV is a statistically significant predictor of uptake of complete (three) doses of the hepatitis B vaccine (p = 0.002) (Table 9).
Discussion
A substantial proportion of respondents interviewed in this survey were aged between 30 and 39 years, followed by 40 – 49 years. This is similar to the findings in the UDUTH Sokoto, Nigeria study,32 but the older age group was predominant in the Uyo Metropolis study (South-South, Nigeria).33 This finding might be because of the lack of recruitment of HCWs into the civil service (Ministry of Health) in Nigeria during the preceding period of this study. In this survey, the mean age of the HCP interviewed was 34.90 ±9.46 years. The presence of this age group, 30 – 39 years in large number in the health sector, could mean having this HCP trained on work-related safety and infection prevention and control practices sector as they may still have a long time to put into the healthcare sector.
Healthcare professional’s knowledge of hepatitis B and hepatitis C
Regarding the two main groups of HCP examined in this study – clinical and non-clinical group, the former expectedly demonstrates a higher level of knowledge of HBV and HCV than the non-clinical related workgroup, and the difference is found to be statistically significant. This is likely because the clinically related workgroup comprised core-health professionals who probably had their infection prevention and control training in their schools/colleges, unlike the non-clinically related group of HCP. All the scientific officers proved to be knowledgeable about HBV and HCV more than the medical doctors, followed by the pharmacist and the laboratory scientists. This finding may be because these scientific officers in this study primarily work in the laboratory unit of the hospital’s Institute of Lassa Fever Research and Control (ILFRC), ISTH Irrua. They have repeatedly undergone some training and retraining in IPC due to the peculiarity of their work which often involves handling samples and specimens of highly infectious diseases.
Uptake and completion of hepatitis B vaccination
In this study, the respondents generally demonstrated poor uptake of the hepatitis B vaccine and a high drop-out rate. This finding of low uptake of hepatitis B vaccine is not consistent with other reports from South-west and South-east Nigeria.34 The uptake rate from the study carried out in South-west Nigeria is higher, while that of South-eastern Nigeria is lower. However, a look at the uptake from other countries of the world clearly shows that the coverage rate in this study is far lower than what others have reported from Burkina Faso (47.7%), Iran (72%), and the United States (75%).15,18,19 These reports from these countries (developing inclusive) could be reflecting the deliberate policy implementation efforts by the government to ensure that hepatitis B vaccination is carried out. Unfortunately, the assessment of hepatitis B vaccination policy amongst HCP goes beyond the scope of this study.
The hepatitis B vaccine drop-out rate from this study is as high as 56% rate. This drop–out rate, although high, is relatively lower than findings from other Nigerian studies, which ranges from 69.6% in Lagos to 83.5% in Enugu.9,12 These previous studies in Niger, however, have a high awareness of hepatitis B vaccination and high drop–out rates. Awareness of vaccination seems not to have translated to better uptake or completing doses of hepatitis B vaccine provisions. Unlike the findings in this study, respondents demonstrated poor knowledge of HBV and HCV with a corresponding low uptake of hepatitis B vaccine. Knowledge requirement for uptake of hepatitis B vaccine may be beyond just the knowledge of the vaccine itself but of the primary blood-borne hepatitis.
A critical appraisal of the reasons for non-uptake and the high drop-out rate is considered in this study. About two-fifths of the respondents said they forgot to go for the next dose of vaccine after the first or second dose. This respondents’ factor is an essential element that should be considered in planning mitigation of the problem. The possibility of employing a reminder system such as calls, alarm systems, and short message services (SMS) may help reduce this large number of drop-outs from completing hepatitis B vaccination. Also, some health system-related factors such as unavailability of vaccine, not being told to come back for the next dose(s), and healthcare workers’ industrial disputes (strikes) are responsible for non-completion in over one-fourth, one-tenth, and one-hundredth of the respondents, respectively. Again, good communication strategies and reminder systems for all those seeking vaccination services could have helped bridge these gaps. Too busy at work was given as a reason for non-completion by one in every 20 respondents. On the other hand, the UDUTH Sokoto (Northwest Nigeria) study reveals about 1 in 100.32 In the Tanzania study, the reasons for non-vaccination were given as: Not being offered vaccine 98 (65.3%) and 60 (41.3%) blamed a low level of awareness regarding the availability of the hepatitis B vaccine.35
In this survey, respondents who did not receive any dose of the hepatitis B vaccine account for about half of the study population. About one–fifth of these respondents stated that they were not aware they had to be vaccinated against hepatitis B. This further highlights the implication of poor knowledge, as earlier stated in this work. As high as about one–fourth of the population gave the non-availability of hepatitis B vaccine as the reason why they never received any hepatitis B vaccine dose. The implication is that some of these HCPs may have been motivated to receive the hepatitis B vaccine, but health system failure led to these missed opportunities. It would have been expected that those who showed up for vaccination were adequately educated. If services are not available, they are politely informed and given the next appointment date to come for vaccination. Again, the different motivations for seeking hepatitis B vaccination services may require strengthening and not being faced with discouraging practices that may make clients never believe in the system or have reasons to come back for another opportunity. In this study, many respondents gave self-motivation as their reason for the hepatitis B vaccine uptake. If their conviction is not very strong, based on sound knowledge and confidence in the system and her services, some of these persons may easily get frustrated and may not come again.
Predictors of uptake and completion of hepatitis B vaccination
The predictors of uptake of at least a dose of hepatitis B vaccine were fair and were statistically associated with working for a shorter duration (1-5 years) and longer duration of 16 -35 years. The predictors of complete uptake of the three doses of hepatitis B vaccine were good knowledge of HBV and HCV. This may be because newly employed staff usually undergo some workplace induction and orientation programme where they are taught the relevant safety protocols and usually encouraged to get vaccinated against hepatitis B infection despite it not being provided by the various hospitals in recent time. In the case of the workers with a work duration of 16-35 years, they probably fall in the category of engaged employees when the policy of compulsory vaccination for all newly employed was in place. As indicated in this study, the main predictor for the completion of hepatitis B vaccination by HCP in the study area is a good knowledge of HBV and HCV. This implies that during workplace orientation for the newly employed HCP and other motivating factors making the HCP commence hepatitis B vaccination, they need to be knowledgeable about HBV and HCV in order to enhance their complete uptake of the hepatitis B vaccine.
Conclusion
The hepatitis B vaccine uptake amongst HCP in this study is low. The HCP demonstrates poor knowledge of HBV and HCV, a significant predictor of hepatitis B vaccine uptake. Duration of work of 1-5 years is a strong predictor of the initiation of the vaccination process. However, there is a high drop-out rate, especially amongst the non-professional group. This rate was mainly due to health system failure (such as non-availability of vaccines and industrial disruption of services) and individual factors such as forgetfulness. Despite the high drop-out rate seen in this study, respondents’ good knowledge of HBV and HCV is a good predictor of completing the vaccination course amongst the HCP who commenced their vaccination uptake.
We would therefore recommend that the immunization unit should ensure regular availability of hepatitis B vaccination commodities and a reminder system like short message services (SMS) or phone calls to inform all HCP desirous of vaccination as well as including lectures on HBV and HCV as part of the CPD for all professional, as hospital seminars for the non-professional HCP in South-South Nigeria. Finally, acceptance and hesitancy factors investigated and identified in the present study could be applied in deriving a better understanding of the uptake and completion of other relevant vaccination programmes in the populace, such as human papilloma vaccination (HPV) or the more recent COVID 19 vaccination.
Declarations
This article is part of a thesis used for the award of Fellow of West African College of Physician in Community Health.
Ethical approval and consent to participate
Ethical approval (Reg. No.:NHREC/29/03/2017) for this study was obtained from the Research and Ethical Committee (HREC) of Irrua Spcialst Teaching Hospital, Irru Edo State, Nigeria. Written informed consent was obtained from all study participants following a thorough explanation of the purposes and dealings of the study, and the benefits were also explained to them. The researchers maintained confidentiality from the inception of the study to the end by ensuring that the administered questionnaires were anonymous and all other means of personal identification were avoided at all times.
Consent for Publication
Not applicable.
Availability of Data and Material
The data from this study will be made available by the corresponding author following a reasonable request.
Acknowledgement
The authors are grateful to members of staff of Irrua Specialist Teaching Hospital, Irrua, Nigeria, for their immense contribution during data collection.
Authors’ contributions
EFO conceived the study and developed the protocol. All authors were involved in the literature review and writing of the manuscript.
Conflict of Interest
There is no conflict of interest.
Funding sources
There is no funding source.
References
- World health organization. Hepatitis B. Fact Sheet No. 204. WHO Media Centre. 2014;204.
- Canadian Centre for Occupational Health & Safety. OSH Answers Fact Sheets. OSH Biological Hazards. Government of Canada; 2016.
- Shepard CW, Simard EP, Finelli L, Fiore AE, Bell BP. Hepatitis B Virus Infection : Epidemiology and Vaccination. Epidemio Rev. 2006;28:112–25.
CrossRef - Zampino R, Boemio A, Sagnelli C, Alessio L, Adinolfi LE, Sagnelli E, et al. Hepatitis B virus burden in developing countries. World J Gastroenterol. 2015;21(42):11941–53.
CrossRef - Agbaji O, Ladep N, Agaba P, Al. E. Prevalence and characteristics of hepatitis B surface antigenaemia among HIV infected patients in Jos, Nigeria. Hungarian Med J. 2008;2:77-82.
CrossRef - Emechebe G, Emodi I, Ikenuna A, Al. E. Hepatitis B virus infection in Nigeria-A review. Niger Med J. 2009;50:18–22.
- Edo State Ministry of Health. Edo State Government: State strategic health development plan (2010-2015). Benin City,Nigeria.; 2010.
- Ogoina D, Pondei K, Adetunji B, Chima G, Isichei C, Gidado S. Prevalence of Hepatitis B Vaccination among Health Care Workers in Nigeria in 2001-2012. The International Occupational Health Journal. 2014;5(1).
- Ibekwe RC, Ibeziako N. Hepatitis B vaccination status among health workers in Enugu, Nigeria. Niger J Clin Pract. 2006;9(1):7-10.
- Fatusi AOA, Esimai AO, Onayade AA, Ojo OSO, Fatusi OA, Esimai AO, et al. Acceptance of hepatitis B vaccine by workers in a Nigerian teaching hospital. East African Medical Journal. 2000;77(11):608–12.
CrossRef - Omokhodion FO. Health and safety in clinical laboratory practice in Ibadan, Nigeria. international Journal of Medicine and Medical Sciences. 1998;27(3–4):201-4.
- Abiola A, Omoyeni OE, Akodu BA. Knowledge, attitude and practice of hepatitis B vaccination among health workers at the Lagos State accident and emergency centre, Toll-Gate, Alausa, Lagos State. West Afr J Med. 2013;32(4):257-62.
- Samuel SO, Aderibigbe SA, Salami TAT, Babatunde OA. Health workers’ knowledge, attitude and behaviour towards hepatitis B infectionin Southern Nigeria. international Journal of Medicine and Medical Sciences. 2009;1(10):421–4.
- Musa BM, Bussell S, Borodo MM, Samaila AA, Femi OL. Prevalence of hepatitis B virus infection in Nigeria, 2000-2013: A systematic review and meta-analysis. Vol. 18, Nigerian Journal of Clinical Practice. 2015. p. 163–72.
CrossRef - Ouédraogo HG, Kouanda S, Tiendrébeogo S, Al. E. Hepatitis B vaccination status and associated factors among health care workers in Burkina Faso. Medecine Et Sante Tropicales. 2013;23:72-7.
CrossRef - Burnett RJ, François G, Mphahlele MJ, Al. E. Hepatitis B vaccination coverage in healthcare workers in Gauteng Province, South Africa. Vaccine. 2011;29:4293-7.
CrossRef - Malewezi B, Omer SB, Mwagomba B, Araru T. Protecting health workers from nosocomial Hepatitis B infections: A review of strategies and challenges for implementation of Hepatitis B vaccination among health workers in Sub-Saharan Africa. Journal of Epidemiology and Global Health. 2016;6(4):229–41.
CrossRef - Simard EP, Miller JT, George P a, Wasley A, Alter MJ, Bell BP, et al. Hepatitis B vaccination coverage levels among healthcare workers in the United States, 2002-2003. Infection control and hospital epidemiology : the official journal of the Society of Hospital Epidemiologists of America. 2007;28(7):783–90.
CrossRef - Moghimi M, Marashi SA, Kabar A, Taghiipour HR, Faghihi-Kashani AH, Ghoddoosi I, et al. Knowledge, Attitude, and Practice of Iranian Surgeons About Blood-Borne Diseases. J Sur Research. 2007;151(1):80–4.
CrossRef - Adekanle O, A Ndububa D, Olowookere S, Ijarotimi O, Ijadunola K. Knowledge of Hepatitis B Virus Infection, Immunization with Hepatitis B Vaccine, Risk Perception, and Challenges to Control Hepatitis among Hospital Workers in a Nigerian Tertiary Hospital. Vol. 2015, Hepatitis research and treatment. 2015. 6 pages.
CrossRef - Kesieme EB, Uwakwe K, Irekpita E, Dongo A, Bwala KJ, Alegbeleye BJ. Knowledge of Hepatitis B Vaccine among Operating Room Personnel in Nigeria and Their Vaccination Status. Hepatitis Research and Treatment. 2011;2011(3):1–5.
CrossRef - Okeke EN, Ladep NG, Agaba EI, Malu AO. Hepatitis B vaccination status and needle stick injuries among medical students in a Nigerian university. Nigerian journal of medicine : journal of the National Association of Resident Doctors of Nigeria. 2015;17(3):330–2.
CrossRef - Adekanle O, Ndububa DA, Olowookere SA, Ijarotimi O, Ijadunola KT, A Ndububa D, et al. Knowledge of Hepatitis B Virus Infection, Immunization with Hepatitis B Vaccine, Risk Perception, and Challenges to Control Hepatitis among Hospital Workers in a Nigerian Tertiary Hospital. Hepatitis research and treatment [Internet]. 2015 Jan 22;2015:439867. Available from: https://doi.org/10.1155/2015/439867
CrossRef - Ogoina D, Pondei K, Adetunji B, Chima G, Isichei C, Gidado S. Prevalence of hepatitis B vaccination among health care workers in Nigeria in 2011-12. The international journal of occupational and environmental medicine. 2014;5(1):51–6.
- Irrua Specialist Teaching Hospital Irrua. Irrua Specialist Teaching Hospital Irrua. ISTH news. ISTH news. 2012;3(3):1–3.
- Registry Department, Irrua Specialist Teaching Hospital I. Category of Staff in ISTH. Irrua, Edo State; 2017.
- Cochran G. Sampling Techniques. 2nd ed. New York: John Wiley and Sons, Inc.; 1963.
- Adedokun B. Sample size determination in Medical Research Methodology. Ibadan: West African College of Physician Research Methodology Update; 2015. p. 1–14.
- Fritzschea C, Beckera F, Hemmera CJ, Riebolda D, Klammta S, Hufertb F, et al. Hepatitis B and C: neglected diseases among health care workers in Cameroon. Transactions of the royal society of tropical Medicine and hygiene [Internet]. 2013 [cited 2016 Mar 26];107(3):158–64. Available from: http://trstmh.oxfordjournals.org/content/107/3/158.abstract
CrossRef - Li X, Kang H, Wang S, Deng Z, Yang T, Jia Y, et al. Knowledge, Attitude, and Behavior of Hepatitis B Virus Infection Among Chinese Dental Interns Xinyi Li, Hengjiu Kang, Shuai Wang, Zhaomin Deng, Ting Yang, Yiping Jia, Yuan Yang Hepat Mon. 2015 May; 15(5): e25079. Published online 2015 May 23. doi: 10.5812. Hepat Mon. 2015;15(5):e25-9.
CrossRef - Osagiede EF, Ozomata EA, Osagiede ET, Jumbo J, Ofanson JE, Abah SO. Assessment of Knowledge and Seroprevalence of Hepatitis B and C Viral Infection among Health Care Personnel in a Rural Teaching Hospital in South-South Nigeria. Journal of Environmental and Occupational Health [Internet]. 2020 [cited 2021 Aug 7];10(3):55–72. Available from: https://www.jenvoh.com/jenvoh-articles/assessment-of-knowledge-and-seroprevalence-of-hepatitis-b-and-c-viral-infection-among-health-care-personnel-in-a-rural-t.pdf
- Hassan M, Awosan KJ, Nasir S, Tunau K, Burodo A, Yakubu A and, et al. Knowledge, risk perception and hepatitis B vaccination status of healthcare workers in Usmanu Danfodiyo University Teaching Hospital , Sokoto , Nigeria. Journal of Public Health and Epidemiology. 2016;8(4):53–9.
CrossRef - Ndako J, Onwuliri E, Adelani-Akande T, Olaolu D, Dahunsi S, Udo U. Screenng for Hepatitis B Surface Antigen (HBsAg) among Health Care Workers (HCW) in an Urban Community, South-South Nigeria. Int J Bio Pharm Allied Sci. 2014;3(3):415–25.
- Omotowo IB, Meka IA, Ijoma UN, Okoli VE, Obienu O, Nwagha T, et al. Uptake of hepatitis B vaccination and its determinants among health care workers in a tertiary health facility in Enugu, South-East, Nigeria. BMC Infectious Diseases. 2018;18(1):1–9.
CrossRef - Aaron D, Nagu T, Rwegasha J, Komba E. Hepatitis B vaccination coverage among healthcare workers at national hospital in Tanzania: How much, who and why? BMC Infectious Diseases. 2017;17(1):2893–8.
CrossRef

This work is licensed under a Creative Commons Attribution 4.0 International License.