How to Cite | Publication History | PlumX Article Matrix
A Systemic Review on Micro-emulsion: Liquid Dosage form for Topical Drug Delivery System
Pratik Dilipraj Dhanawate1 , Ashwini Ramkrishana Gawade2*
, Ashwini Ramkrishana Gawade2* , Ashwin Bhanudas Kuchekar2
, Ashwin Bhanudas Kuchekar2  and Akash Anil Podutwar2
and Akash Anil Podutwar2
1MAEER’s Maharashtra Institute of Pharmacy, Savitribai Phule Pune University, Kothrud Pune, Maharashtra, India.
2School of Pharmacy Dr. Vishwanth Karad MIT World Peace University, Kothrud, Pune, Maharashtra, India.
Corresponding Author E-mail: ashwinigawade890@gmail.com
DOI : http://dx.doi.org/10.13005/bbra/3005
ABSTRACT:
Microemulsions (ME) is a system that combines water, oil, and an emulsifier / surfactant which is a form of volatile liquid, homogeneous and kinetically stable. Microemulsion is an attractive drug delivery system for topical administration. Due to its solubility, mild skin irritation, and watery swelling are used in the Topical Drug Delivery System (TDDS). By improving the quality of skin texture, it provides a level of penetration. The function of skin balance is to limit the penetration of bacteria, viruses, and other environmental factors. With standard drugs, skin penetration may take time and have not been able to provide immediate action. So, in this case, we used the Microemulsion-based Topical Drug Delivery system. Microemulsion increases solubility, protects the drug from environmental factors and improves drug bioavailability. MEs provide high penetration and the ability to penetrate into the skin. Because of this, the immediate action of the drug can occur in the infected area. Due to the presence of a hydrophilic and lipophilic environment, it provides outstanding biocompatibility. There are several test frames used to maintain stability, microemulsion kinetics.
KEYWORDS: Biocompatibility; Microemulsion; Skin Penetration; Topical Administration
Download this article as:| Copy the following to cite this article: Dhanawate P. D, Gawade A. R, Kuchekar A. B, Podutwar A. A. A Systemic Review on Micro-emulsion: Liquid Dosage form for Topical Drug Delivery System.Biosci Biotech Res Asia 2022;19(2). |
| Copy the following to cite this URL: Dhanawate P. D, Gawade A. R, Kuchekar A. B, Podutwar A. A. A Systemic Review on Micro-emulsion: Liquid Dosage form for Topical Drug Delivery System.Biosci Biotech Res Asia 2022;19(2). Available from: https://bit.ly/3wFktRb |
Introduction
Topical Drug Delivery System (TDDS) has been commonly used in the field of cosmetics. It will be used for the treatment of dermal infections caused by bacteria are acne, pimples, cellulitis, fungal infection are Tinea corporis, Tinea pedis, Tinea barbae candidiasis, dermatophytosis. For the treatment of this infection, we used the topical drug delivery system1. In the TDDS drug can be delivered directly onto the infected area or a body surface. There are many common topical medications available in the market such as ointment, lotion, gels, powders, and transdermal patches. In the topical drug delivery system (TDDS) drugs can be applied on skin that was present interiorly (mouth portion, rectal route) and also the exterior part of the body (Skin)2. TDDS have a local effect and also a systemic effect when 2drugs reach the body’s circulation system after application to the dermis. TDDS has a very fast local action on the application area or the part of the body where we applied3. Topical medication had a serious effect on the body for avoiding it used by taking the advice of a physician. Otherwise, a topical drug delivery system is a very useful and easy technique for the administration of the drug, cause in this technique the self-administration of the drug is possible. This technique avoids 1st pass hepatic metabolism and the enzyme degradation Gastrointestinal Tract and also avoids gastrointestinal irritation4. TDDS is an alternate route for those who are unable to take oral medications. This drug delivery system is not affected by vomiting or diarrhea5. In TDDS drug administration is stopped by removing the patch. TDDS is generally used when the other system of drug administration fails or is mainly used in dermal infection. For its instant action or effect, the drug has to be penetrated through all the three main dermal layers, but the most important and initial penetration is through the horny layer(stratum corneum) which acts as a limiting barrier for the drugs6. After this, the drug has been passing through the deeper epidermis and dermis without drug accumulation in all three dermal layers. However, for enhancing the local or systemic effect of the drug we used emulsion-based drugs. Emulsion-based drugs increase the ability of penetration and permeation through the skin. The classification of emulsion is shown in the figure.1.
 |
Figure 1: Emulsion Types |
The emulsions are liquid dosage forms in which the dispersed phase is composed of tiny globules of a liquid distributed throughout a vehicle in which it is immiscible7. All emulsions are innately unsteady systems due to the thermodynamic incompatibility of the oil and water phases at the interface8. Continuous and dispersed are the two phases present in the emulsion. In this when water is in the dispersed phase then the oil is in the continuous phase and vice-versa. Surfactant or “surface-active agents” is a broader group and the most important part of emulsion also known as emulsifiers9. Surfactants are nothing but amphiphilic compounds, which means they have a hydrophilic part/ polar (water-soluble) and lipophilic part /non-polar (oil soluble). Because of the amphiphilic nature, surfactants tend to have less or more solubility either in oil or water. Moreover, emulsion molecules have a bimolecular nature (hydrophilic, lipophilic), because of this, they have more penetration and permeation capacity to the skin10. The emulsion had a cloudy appearance only because these many phases interface the scattering of light as it passed through the emulsion. When all light is scattered equally, it appears white.
Microemulsion for Transdermal Drug Delivery System
Microemulsions (ME) is a system composed of water, oil, and emulsifier/surfactant which is an optically isotropic and kinetically stable liquid solution. ME is an innovative drug delivery system composed of the oil phase, surfactant, aqueous phases, and co-surfactant and has been used to improve the rate and absorption of lipophilic drugs. Due to its solubility, mild skin irritation, and inflated permeability is used in the TDDS. By improving the quality of the dermal formulation, it provides the extent rate of permeation. ME improves the solubility of drugs, unstable drugs will be protected against the environmental condition, it enhances the bioavailability of the drug, and increases the shelf life11. The microemulsion is an economical and convincing drug carrier system that delivers the drug successfully onto all over the skin. MEs had good formulation properties, their ability to intensify the penetration of hydrophilic and hydrophobic drugs, and outstanding biocompatibility onto the dermis due to the presence of the hydrophilic and lipophilic nature. Microemulsions are the clear homogeneous and thermodynamically stable system in which the droplet size range is from 0.1-.1.0μm. There are number of mechanisms had reported explaining that microemulsion advantages as used in TDDS. A large amount of drug that can be assimilated into a ME due to its better solubilizing capacity can increase the kinetic activity of a drug towards the skin. It enhances the thermodynamic activity of the dugs that causes may an improvement in the partitioning of the skin. The ingredients of microemulsion may affect the layer stratum corneum. Due to microemulsion, the permeation ability may be influenced by the drug on the stratum corneum layer. The formulation is influenced by the hydration effect of MEs on the stratum corneum. Due to the low viscosity of the MEs, it was a challenge to administer as a solution onto the skin. Moreover, for optimization of the ME in the transdermal formulation, we have to use the different gels (carbomer, xanthan gum, carrageenan). A gel is a cross-linked hydrophilic polymer that swell and hold a lot of water at the same time maintaining the structure by physical or chemical crosslinking of individual polymer chains and studies show that the hydrogel enhances the viscosity of microemulsion12. Microemulsion (ME)is an appealing drug delivery system for topical administration. ME can form the proper ratio of the water, oil, and surfactant and the formation of it requires low energy13. In MEs droplet is in nano-size and liquid is clear. Emulsifiers in ME help to penetrate the skin and the aqueous phase contributed to the moistening of the skin. These parameters offered by MEs will increase the chances of drug penetration into deeper layers of the dermis than regular topical formulations can.
Formulations of Microemulsions
Micro-emulsion is stable clear and isotropic mixture of oil, water, surfactant, and sometimes co-sufactant14. Surfactant had a hydrophilic and lipophilic property which balances the by continuous type of emulsion.
The following ingredients used in the formulation of microemulsion are shown the table 1.
Table 1:Containts of Microemulsion.
| SR. NO. | Ingredient | Type | Example |
| 1 | Oil Phase | LCTs
Mono/Di-glyceride Fatty Acid
|
Soybean oil, Olive oil, cottonseed oil.
Glyceryl caprylate/caprate Oleic acid |
| 2 | Surfactant | Cationic,
Anionic, Non-Ionic
|
Quaternary ammonium salts.
Sulfate, Sulfonate. Polyoxyethylene surfactant, Span. |
| 3 | Co- Surfactant | Short-chain alcohol,
Alkane diols and triols, Organic acid and salt |
Ethanol, benzyl alcohol.
Glycerol, butylene glycol. Caprylic acid, Sodium Caprylate. |
| 4 | Aqueous Phase | – |
Water, Different buffers. |
Importance of Microemulsions
Microemulsion enhances drug solubility and thermodynamic activity toward the skin enhances permeation activity of its components, is easy to formulate, and fosters the system’s thermodynamic stability. Microemulsions are known to increase the absorption of the applied drug at the site of application. The reason for this is the penetration enhancement effect of the carrier, mostly composed of saturated as well as unsaturated fatty acids as the oil phase. Reduction in dose quantity due to high bioavailability.
However, microemulsions suffer from high surfactant concentrations and in most cases from high alcohol, solvent, and co-solvent contents.
Theory of Formulation of Microemulsion
For the formulation of the microemulsion, there are three important theories proposedare-
Thermodynamic theory.
Mixed/ Interfacial film theory.
Solubilization theory.
Thermodynamic theory
In this the free energy for the formation of MEs depends on surfactant which helps in lowering the surface tension on the oil-water interface and change in entropy of the system such that the,
∆G = γ∆A – T∆S
∆G is free energy formation, is the surface tension of the oil-water interface, T the temperature, is the entropy change and the is increased due to formation of a hugenumber of tiny droplets are formed in ME15.
Interfacial film theory
Due to formed droplets of the microemulsion, film of the water-oil interface formed by the surfactant and co-surfactant. This film is presumed that to be consist of a two-part film of MEs formed depending curve of the interface.
Solubilization theory
It illustrates the relationship between the W/O microemulsion and micelles by using the phase diagram. In this, micelles solubilized the oil and aqueous phase. Microemulsions solubilized by the reverse micelles.
Surfactant helps in the formation of ME and reduces the interfacial tension of microemulsion.
The selection of surfactants will be done based on the hydrophilic-lipophilic balance (HLB) concept and the critical packing parameter concept. For the formation of the W/O MEs used the surfactants with a Low HLB value range (3-6), and for the O/W MEs used the surfactant with a High HLB value range (8-18)16.
Skin Anatomy
Skin covers the entire external body surface and is known as the cutaneous membrane. The thickness of skin differs from person to person and the pH of the skin range from the 4 to 5.6. The largest organ of the body in weight and surface area17.
Skin
Area covers- 2sq.m.
Weighs – 4.5-5 kg 9(7-8% of total body weight).
The skin comprises of two major parts. The outermost part is known as the epidermis and the deeper part is known as the dermis. The epidermis is a thinner portion and composed of epithelial tissues. While the dermis is a thicker portion and composed of the connective tissues. The hypodermis is present deep to the dermis but is not part of the skin, this layer composed of the adipose and areolar tissue. Melanocytes, Langerhans cells, Merkel cells and Keratinocytes cells are the 4 principle types of cells that carry the epidermis18. Stratum germinativum, Stratum granulosum, Stratum spinosum, and stratum corneum (horny layer) these four strata are present in the epidermis layer in most of the regions of the body. But in between all of them, there is most important layer is the stratum corneum. This layer is composed of flat keratinocytes contain at most of the keratin and 35-30 rows of dead cells. It functions to protect the deeper layers from injury and microbial invasion. In this layer, the arrangement of the cell membrane is complex, with wavy folds to hold the layer together with adjacent cells19. For the drug penetration through the layer stratum corneum is a tough job for this we used ME based drug delivery system.
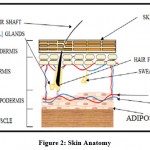 |
Figure 2: Skin Anatomy. |
Routes of Drug Permeation through Skin
Delivery of the drug through the skin layer is done painlessly. Increasing the efficacy of the TDDS route is depends on the penetration ability of that drug. The formulation type and physicochemical properties of the drugs are factors responsible for the efficacy of the transdermal route20. Firstly, the drug has to be passed through the primary barrier of the skin stratum corneum. For enhancing the permeation there are some routes for the drugs that are21:
Intercellular route: use for the hydrophilic drug.
Follicular route: mediate delivery of the various drug.
Intracellular Route: use for the lipophilic drug.
For increasing the drug permeation through the dermis/skin we have to use a suitable carrier system. To do this, the microemulsions are the potential drug carrier system or the topical also for the transdermal. MEs increase the drug transfer over the dermis/skin and bypass the horny layer. This happened because the MEs are thermodynamically stable and clear dispersion of two liquid phases. Dispersion of two liquid phases is stabilized by the mixed film of emulsifier and co-surfactant. MEs provide high permeation to the drug because they have minimum surface tension and droplet size22.Droplet size in ME is less than 0.1μm.Microemulsions are inadequate to reflect the light and are invisible when we observe them under the optical microscope. The ternary phase diagram is used for representing MEs. All 3 edges of the ternary phase diagram show the water, oil, and surfactant, as shown in the figure. 3.
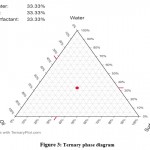 |
Figure 3: Ternary phase diagram. |
Despite extensive research and positive effects on the potential of microemulsions as skin delivery systems, studies have been designed to investigate advanced drug delivery methods from microemulsions. The first possible hypothesis considered a large dose of microemulsion drug as possible as it could provide higher concentration and thus increase the driving capacity of the skin23. This process is possible but may not be the only method that works as it could explain improved delivery of lipophilic drugs but not hydrophilic drugs that do not have a melting problem. The second possibility is to assume that the effect of enhancing the penetration of microemulsion components is responsible for improved skin delivery from microemulsion. This process is supported by the fact that most oils, surfactants and cosurfactant are known to have an enhancing effect. A third possibility depends on the penetration of microemulsion elements into the skin as monomers and the effect that the solubility of the drug on the skin increases. This will increase the secretion of the drug on the skin, create a high drug density within the upper parts of the skin and thus have a greater driving force in the delivery of the dynamic drug. This procedure is supported by the findings of Hathout et al., who documented the collection of microemulsions in lipid intercellular domains. The fourth method looks at the possible direct transfer of the drug from the microemulsion droplet to the stratum corneum. This consideration depends on the presence of the drug in the microstructure of the microemulsion, which has a very small droplet size, which provides a large area for drug transfer to the skin. The fifth possible method using very low surface friction will provide excellent distribution and interaction between the microemulsion and the skin. This will allow the car to fill up even wrinkles and small cracks in the skin to facilitate the transfer of the car skin to the car. This condition is supported by findings that reflect the height of a cosurfactant-containing system in addition to the free cosurfactant system as the cosurfactant is known to provide a continuous reduction in facial tension. The sixth method relies on the feasibility of an in situ supersaturation process that will increase thermodynamic activity and the driving force of transdermal drug transfer. Supersaturation can be obtained by immediately applying nonsolvent to a drug solution. This will create a solution where the concentration of the drug exceeds the melting point. A possible last resort may depend on improved penetration into the follicle24. This may be supported by a double increase in drug trans-follicular penetration after the application of microemulsion or liposomes compared to most traditional coarse emulsions. These findings provide potential benefits in the treatment of acne vulgaris and require further clinical investigation to confirm or refute this theory.
Mechanism of action of drug Permeation Enhancer
For increasing the drug permeation through the skin, we have to increase the percutaneous absorption. For this, the new strategies are adapted such as the vehicle system, drug carrier system, permeation enhancer, or transdermal patches. By using all these techniques, we can temporarily destruct the layer stratum corneum. MEs reduce the interfacial tension and surfactant or lipid increases the permeation. During this, surfactant or emulsifier may dissolve the phospholipid bilayer structure of the horny layer. Moreover, by minimizing the horny layer, the pores or passage for the drug transfer are opened25. The arrangement of the phospholipid bilayer and keratinized cells of the stratum barrier alter by the penetration enhancer. The interaction is explained by the Lipid –Protein Partitioning theory: – Three main mechanisms suggest in this theory.
According to this theory,
Drug interacts with the intercellular lipid bilayer membrane.
Then, interacts with keratinized cells.
And the result is drug penetrates the phospholipid bilayer of the horny layer.
After the barrier gets minimized, drug diffusion takes place through above mentioned significant pathways.
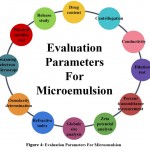 |
Figure 4: Evaluation Parameters For Microemulsion. |
Conclusion
The drug-filled with the microemulsion-based drug delivery system is effectively used in the topical drug delivery system (TDDS). It is an alternative option of the dosage forms like oral, intravenous. The TDDS ensures that an active pharmaceutical substance arrives at a relevant location with minimal side effects. The research and study show that the microemulsion can be used in the topical drug delivery system. By using the MEs in TDDS it will give instant action on that location where we applied. The microemulsion can protect the drugs, enhance the solubility of a drug, and have good penetration and permeation capacity towards the skin. Furthermore, a micro emulsion-based TDDS has very few side effects occurs and more acceptances from the patients. But also, the recent formulations of MEs can retain the drugs for extended periods.
Acknowledgement
Authors are thankful to the faculty of MAEER’s Maharashtra Institute of Pharmacy, Savitribai Phule Pune University and School of Pharmacy, Dr Vishwanath Karad MIT World Peace University, Pune, Maharashtra, India for their guidance and for allowing me to write this review article.
Conflict Of Interest
The author declares there is no conflict of interest.
Funding Sources
There is no funding source.
References
- Goswami P, Choudhury A, Dey BK. Microemulsion- A potential carrier for improved bioavailability. J. Inernational Journal of Pharmceutical and Biological Archieves. 2019;10(2):69-77.
- Azizi M, Esmaeili F, Partoazar A, Ejtemaei Mehr S, Amani A. Efficacy of nano- and microemulsion-based topical gels in delivery of ibuprofen: an in vivo study. J Microencapsul. 2017;34(2):195-202.
CrossRef - Das S, Lee SH, Chia VD, et al. Development of microemulsion based topical ivermectin formulations: Pre-formulation and formulation studies. Colloids Surfaces B Biointerfaces. 2020;189(October 2019):110823.
CrossRef - Froelich A, Osmałek T, Snela A, et al. Novel microemulsion-based gels for topical delivery of indomethacin: Formulation, physicochemical properties and in vitro drug release studies. J Colloid Interface Sci. 2017;507:323-336.
CrossRef - Leppert W, Malec-Milewska M, Zajaczkowska R, Wordliczek J. Transdermal and topical drug administration in the treatment of pain. Molecules. 2018;23(3):1-16.
CrossRef - Chauhan L, Thakur P, Sharma S. Microemulsions : New vista in novel drug delivery system. Innov Pharm Pharmacother. 2019;7(2):37-44.
- Kale S, Deore S. Emulsion Microemulsion and Nanoemulsion. Syst Rev Pharm. 2017;8(1):39-47.
CrossRef - Hajjar B, Zier KI, Khalid N, Azarmi S, Löbenberg R. Evaluation of a microemulsion-based gel formulation for topical drug delivery of diclofenac sodium. J Pharm Investig. 2018;48(3):351-362.
CrossRef - Callender SP, Mathews JA, Kobernyk K, Wettig SD. Microemulsion utility in pharmaceuticals: Implications for multi-drug delivery. Int J Pharm. 2017;526(1-2):425-442.
CrossRef - Choudhury H, Gorain B, Pandey M, et al. Recent Update on Nanoemulgel as Topical Drug Delivery System. J Pharm Sci. 2017;106(7):1736-1751.
CrossRef - Egito EST, Amaral-Machado L, Alencar EN, Oliveira AG. Microemulsion systems: from the design and architecture to the building of a new delivery system for multiple-route drug delivery. Drug Deliv Transl Res. 2021;11(5):2108-2133.
CrossRef - Patil P., Datir S., Saudagar R. A Review on Topical Gels as Drug Delivery System. J Drug Deliv Ther. 2019;9(3):661-668.
CrossRef - Paliwal H, Solanki RS, Chauhan CS, Dwivedi J. Pharmaceutical Considerations of Microemulsion as a Drug Delivery System. J Drug Deliv Ther. 2019;9(4):661-665.
- Pal S, Prajapati RN, Pateriya K, Bijauliya RK. a Review on Microemulsion Based Drug Delivery System. IJRAR-International J Res Anal Rev. 2019;6(1):682-689.
- Ita K. Progress in the use of microemulsions for transdermal and dermal drug delivery. Pharm Dev Technol. 2017;22(4):467-475.
CrossRef - van Staden D, du Plessis J, Viljoen J. Development of a self-emulsifying drug delivery system for optimized topical delivery of clofazimine. Pharmaceutics. 2020;12(6):1-24.
CrossRef - Ashara KC, Paun JS, Soniwala MM, Chavada JR, Mori NM. Micro-emulsion based emulgel: A novel topical drug delivery system. Asian Pacific J Trop Dis. 2014;4(S1).
CrossRef - Zhou X, Hao Y, Yuan L, et al. Nano-formulations for transdermal drug delivery: A review. Chinese Chem Lett. 2018;29(12):1713-1724.
CrossRef - Jiang T, Wang T, Li T, et al. Enhanced Transdermal Drug Delivery by Transfersome-Embedded Oligopeptide Hydrogel for Topical Chemotherapy of Melanoma. ACS Nano. Published online 2018.
CrossRef - Benson HAE, Grice JE, Mohammed Y, Namjoshi S, Roberts MS. Topical and Transdermal Drug Delivery: From Simple Potions to Smart Technologies. Curr Drug Deliv. 2019;16(5):444-460.
CrossRef - Article R. Microemulsions : Transdermal Drug Delivery Systems with Enhanced. 2019;9:835-837.
- Scomoroscenco C, Teodorescu M, Raducan A, et al. Novel gel microemulsion as topical drug delivery system for curcumin in dermatocosmetics. Pharmaceutics. 2021;13(4).
CrossRef - Al-Adham ISI, Jaber N, Al-Remawi M, et al. A review of the antimicrobial activity of thermodynamically stable microemulsions. Lett Appl Microbiol. Published online 2021:1-11.
CrossRef - Nastiti CMRR, Ponto T, Abd E, Grice JE, Benson HAE, Roberts MS. Topical nano and microemulsions for skin delivery. Pharmaceutics. 2017;9(4):1-25.
CrossRef - Desmet E, Van Gele M, Lambert J. Topically applied lipid- and surfactant-based nanoparticles in the treatment of skin disorders. Expert Opin Drug Deliv. 2017;14(1):109-122.
CrossRef

This work is licensed under a Creative Commons Attribution 4.0 International License.





