How to Cite | Publication History | PlumX Article Matrix
Mohammad Irfan Abdul Kader1* , V. Karthikeyan1
, V. Karthikeyan1 and Sabitha J2
and Sabitha J2
1Department of Pharmacy Practice, Grace College of Pharmacy, Kodunthirapully, Palakkad, Kerala- India
2Gynaecologist-Obstetrician, Paalana Institute of Medical Sciences, Palakkad, Kerala- India
Corresponding Author E-mail:muhammedirfanea@gmail.com
DOI : http://dx.doi.org/10.13005/bbra/3115
ABSTRACT: Background: Dysfunctional uterine bleeding (DUB) is defined as bleeding from the uterine corpus that is abnormal in regularity, volume, frequency, or duration and occurs in the absence of pregnancy. Methylprogesterone (MPA) and Norethisterone (NE) are a sort of female hormone (progestin).To cure dysfunctional uterine bleeding, this study sought to determine how MPA and NE worked. Materials and Procedures Over three months, a prospective observational study was conducted at a hospital in Palakkad. The usefulness of MPA and NE is analyzed by using the PBAC score method. Using Microsoft Excel 2007, the cases were entered, and descriptive statistical analysis was then performed. Results and Discussion There were 71 respondents in this study, with ages ranging from 18 to 35 and older. 32 of the 71 people received MPA, whereas 39 of them acquired NE. DUB was much more prevalent in women over 35 (NE-56.4% and MPA-75%). DUB is usually seen in overweight individuals (NE: 56.4%; MPA: 50.). The PBAC score dropped after both medications were administered. Norethisterone is more effective than either of the drugs, as per this study.
KEYWORDS: Dysfunctional Uterine Bleeding (DUB); Medroxyprogesterone (MPA); Norethisterone (NE); Pictorial Blood Assessment Chart (PBAC)
Download this article as:| Copy the following to cite this article: Kader M. I. A, Karthikeyan V, Sabitha J. A Comparative Study on Efficacy of Norethisterone and Medroxyprogestrone in the Management of Dysfunctional Uterine Bleeding: A Prospective Observational Study. Biosci Biotech Res Asia 2023;20(2). |
| Copy the following to cite this URL: Kader M. I. A, Karthikeyan V, Sabitha J. A Comparative Study on Efficacy of Norethisterone and Medroxyprogestrone in the Management of Dysfunctional Uterine Bleeding: A Prospective Observational Study. Biosci Biotech Res Asia 2023;20(2). Available from: https://bit.ly/3NTgvgC |
Introduction
Dysfunctional Uterine Bleeding (DUB) is defined as abnormal uterine blood loss in the absence of organic genital tract disease. It refers to any variation in uterine bleeding, including menstrual cycle disturbances, rhythmic and non-rhythmic uterine bleeding, and revision in the amount or duration of menstruation loss. However, it tends to most generally refer to excessive normal menstrual bleeding or vital menorrhagia. 1 Either it may be acute or chronic, acute AUB is a kind of bleeding that affects women of reproductive age and necessitates prompt treatment to stop future blood loss. Contrarily, chronic AUB is uterine corpus bleeding that has been present for the previous six months and is of abnormal duration, severity, or recurrence.2 The pathophysiology of DUB cannot be understood without first understanding what is “normal” and “abnormal.” Bleeding beyond the typical range of 28 days (+/- 7 days) between menstrual cycles is abnormal. The follicular phase is the term used to describe the first half of the menstrual cycle. The amount of estrogen is gradually increasing at this stage. Ovulation takes place on day 14 and the luteal phase starts. The corpus luteum, which generates progesterone to counteract estrogen, is nestled inside the ovum. In the absence of fertilization, progesterone, and oestrogen levels begin to fall, the endometrial lining breaches, and menstruation results.3, 4 Menstrual bleeding typically lasts 4 days. An average of 35 mL of blood are lost throughout each period. 80 mL or less of total menstrual blood loss per period is considered abnormal.5
DUB may indeed arise from a systemic condition, organic anomaly (such as fibroids), or functional aberration (e.g., von Willebrand disease).6 The prevalence differs depending on the region and spans from 10 to 30 %. AUB prevalence in India is currently estimated to be 17.9%.7
Medroxyprogesterone is a specific kind of female hormone (progestin). This drug is analogous to the progesterone our systems naturally produce. It is used to treat abnormal uterine bleeding, amenorrhea, is also used in palliative care for endometrial and renal carcinoma.8,9 it prevents follicular maturation and ovulation by inhibiting the synthesis of gonadotropin, which is what gives it the capacity to prevent pregnancy. The endometrium is also thinned by this activity. In endometrial epithelial cells, MPA decreases DNA synthesis and nuclear oestrogen receptors.10 Oral medroxyprogesterone acetate (MPA) has a biological half-life of 40–60 hours and an absorption half-life of 15–30 minutes.10, 11
Norethisterone, is a progestin drug used to treat gynaecological problems, menopausal hormone treatment, and birth control medications.12 it acts on target cells by attaching to progesterone receptors, which causes alterations in the target genes downstream. It also causes an array of endometrial alterations that render the tissue unsuitable for implantation, such as atrophy, erratic secretion, and inhibited proliferation.14 Norethisterone’s half-life has been variously estimated to be 8–10 hours.14
Menstrual Blood Loss is evaluated using a semiquantitative method called a pictorial blood loss assessment chart (PBAC). This straightforward, reasonably priced instrument features a visual grading system that displays a graded series of soiled towels and/or tampons. The patient can keep a direct record of how many used pads/tampons she has and how heavily stained they are with blood.15
Materials and Method
The present study was a prospective observational study, conducted at Paalana Institute of Medical Sciences, a multi super- specialty hospital that is well equipped and has a capacity of more than 250 beds. The study period was from July 2022 to December 2022 (6 months). The study was approved by Institutional Ethics Committee GCP/IEC/112E/2022 dated 05-07-2022. The Inclusion Criteria were female patients aged >18 years attending the gynaecology department. Patients with Heavy Menstrual Bleeding, no drug abuse in the last six months, no coagulation disorders, and no history of Cardiac surgery in the last 3 months. Exclusion Criteria were patients with a History of Hormone therapy in the previous 3 months, Patients not willing to give consent for the study, and patients with Progestin drug allergy. The study was explained to patients and written informed consent was taken from patients. A pre-designed patient data collection form is used to collect the required information, regarding the patient’s demographic details, past medical and medication history, detailed social habits, reproductive history, signs and symptoms, laboratory investigations, sonographic findings, and treatment chart .it also includes the general required information such as age, body weight, BMI, occupation, and educational level; daily living habits such as the frequency of drinking sweet drinks and eating sweet foods, the frequency of exercise, the previous history of any contraceptive methods, reproductive history such as marriage state, etc. The patients were divided into two groups, those who were taking NE as group 1 and taking MPA as group 2. The two drugs are given randomly to the two groups in specific doses, frequency, and duration (NE- 5mg × 25 days) (MPA – 10mg × 21 days). To assess the amount of blood flow PBAC score was evaluated. They noted how many napkins are used in a cycle. Also observed the quantity and size of the passed clots. The patients were asked to use sanitary pads of similar absorbent capacity. Scores were assigned to a different degree of soiling of sanitary napkins, number and size of clots passed.
The PBAC score was calculated by assigning a sanitary pad a score of 1, 5, or 20 depending on how unclean it was, and a score of 1 or 5 depending on whether it had passed little or big clots. A sparse flow is considered to be one with a PBAC score of 10 or below. 10-100 is regarded as moderate flow, 300 or more is very severe flow, and 100 to 300 is severe flow. When the PBAC score is larger than 100, blood loss of much more than 80 ml defines as diagnostic menorrhagia. When a towel or tampon was discarded, the women were asked to place a mark in the appropriate box; if there were enough, they were recorded in groups of five. 16 Patients were requested to fill out a fresh menstrual record each month before their three-month follow-up visits, which included a gynaecological exam and an assessment of their PBAC score, in order to track the impact of therapies on menstrual blood loss. The instances were then loaded into MS Excel 2007 to determine the proportion of different parameters. Descriptive statistics like frequency and percentage are used to describe the demographic characteristics and determinants of DUB.
Result
Table 1: Prevalence Distribution Based on Specific Drugs
|
Sl. No. |
Specific drugs |
No. of patients |
Percentage (%) |
|
1 |
Norethisterone |
39 |
54.9 % |
|
2 |
Medroxyprogesterone acetate |
32 |
45.07 % |
A total of 71 cases were included, among them, 54.9% of the (n=39) cases were under the Norethisterone group and 32 cases were under the Medroxyprogesterone group. As more patients were seen under the Norethisterone treated group.
Table 2: Prevalence Distribution of Women Based on Age Category
|
Sl. No. |
Age groups (in years) |
NE |
MPA |
||||
|
No. of patients (n=39) |
Mean age ±SD |
Percentage (%) |
No.of patients (n=32) |
Mean age ±SD |
Percentage (%) |
||
|
1 |
18-35 |
10 |
28.5±3.3 |
25.7% |
8 |
29.3±3.1 |
25% |
|
2 |
>35 |
29 |
44.4±5.6 |
74.3% |
24 |
46.6±5.1 |
75% |
Among the collected cases, In the NE group, 74.3%% of patients were under the age category >35 years followed by 25.7% under 18-35 years.
In the MPA group, 75% of patients were under the age category >35 years followed by 25% under 18-35 years. Based on the data, DUB was more prevalent among the age group > 35 years in both groups. As we interpret the data the DUB increases with increasing age.
Distribution Based on Socio-Demographic Characteristics
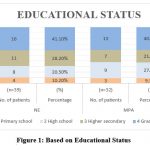 |
Figure 1: Based on Educational Status
|
Based upon the Educational status, In the NE group, about 41.1% of the patients were graduates, 28.2% of the patients are having higher secondary education, and 20.5% of the patients with high school education followed by 10.2% had primary school education.
In the MPA group, about 40.6% of the patients were graduates, 21.8% of the patients had higher secondary education, and 27.9% of the patients with high school education followed by 9.3% of the patients having primary school education. Based on this data, the type of counseling for the patient was prepared ie; whether it should be in the local language or professional manner.
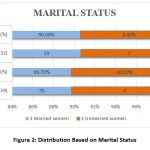 |
Figure 2: Distribution Based on Marital Status.
|
Based on marital status, In the NE group, 89.7% of the patients were in the Married women category followed by 10.3% of the patients in the Unmarried women category
In the MPA group, 90.6% of the patients were in the Married women category followed by 9.4% of the patients in the Unmarried women category. So in both groups, DUB is more prevalent among the Married women category. Married women mostly have changes in their hormone due to intercourse and delivery. So the chances of DUB are more in married women.
Table 3: Distribution Based on BMI
|
Sl. No |
BMI (Kg/m2) |
NE |
MPA |
||||
|
No. of patients (n=39) |
Mean BMI ±SD |
Percentage (%) |
No. of patients (n=32) |
Mean BMI ±SD |
Percentage (%) |
||
|
1 |
<18.5 (Underweight) |
2 |
16.9±0.4 |
5.1% |
4 |
16.9±0.5 |
12.5% |
|
2 |
18.5-24.9 (Normal) |
12 |
21.5±1.4 |
30.7% |
9 |
21.1±1.4 |
28.1% |
|
3 |
25-29.9 (Overweight) |
22 |
26.6±1.3 |
56.4% |
16 |
26.6±1.3 |
50.1% |
|
4 |
>29.9 (Obesity) |
3 |
31.2±1.1 |
7.6% |
3 |
31.8±1.1 |
9.3% |
Based on Body Mass Index (BMI), In the NE group, 56.4% of patients were under the overweight category (25-29.9), 30.7% of patients were under the normal category (18.5-24.9),7.6% of patients under obesity (>29.9%) followed by 5.1% patients under underweight category(<18.5).In the MPA group, 50.1% of patients were under the overweight category (25-29.9), 28.1% of patients were under the normal category (18.5-24.9),12.5% of patients under the underweight category(<18.5)followed by 9.3% patients under obesity (>29.9%) Prevalence of DUB is higher in women with BMI ranging between 25-29.9 ie; 56.4% in NE group patients and 50.1% in MPA group patients, which indicate overweight is also a reason for developing DUB. The overweight indicates an abnormality in the lipid profile, which greatly affects the hormonal balance, as it increases the chance of DUB.
Table 4: Distribution Based on BMI
|
Mean Hb level (gm %) |
|||
|
|
Pretreatment |
After therapy |
p value |
|
Norethisterone (n=39) |
8.2 |
10.6 |
0.0002 |
|
Medroxyprogestrone (n=32) |
8.3 |
10.2 |
|
As for the hemoglobin level, In the NE group – The Mean Hb value at the baseline was found to be 8.2g% and after the treatment, the mean Hb was found to b 10.6g% (p<0.0001) In the MPA group – The mean Hb value at the baseline was found to be 8.3g% and after the treatment, the mean Hb was found to b 10.2g% (p<0.0001). On comparing both the groups, the rise in hemoglobin level was more with norethisterone and the difference was statistically significant (p<0.0002). As in DUB patients, the chance of reduction of Hemoglobin is significant, in most cases, the patient will become anemic. As the treatment has been taken properly, the hemoglobin level will also get raised.
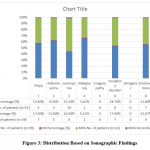 |
Figure 3: Distribution Based on Sonographic Findings
|
Based on the collected data, In the NE group – 9 patients (23%) were affected with endometriosis, 8 patients (20.5%) were affected with leiomyoma, 7 patients (17.9%) were affected with a polyp, 7 patients (17.9%) affected with an ovulatory disorder, 5 patients (12.8%) affected with adenomyoma and 2 patients (5.1%) affected with malignancy. In the MPA group – 10 patients (31.2%) were affected with leiomyoma, 7 patients (21.8%) were affected with endometriosis, 6 patients (18.7%) were affected with an ovulatory disorder, 5 patients (15.6%) were affected with a polyp, 3 patients (9.3%) affected with adenomyoma and 1 patient (3.1%) affected with malignancy. All conditions mentioned above will cause abnormality in uterine bleeding, it is because of changes in the anatomy of the uterus.
Table 5: Distribution Based on PBAC Score
|
Mean PBAC score |
|||
|
|
Pretreatment |
After therapy |
p value |
|
Norethisterone (n=39) |
230 |
96 |
< 0.0001 |
|
Medroxyprogestrone (n=32) |
226 |
113 |
|
Based on the collected data, In the NE group, Mean PBAC at the baseline was found to be 230 and after treatment Mean PBAC was decreased to 96 (p <0.0001).
In the MPA group, Mean PBAC at the baseline was found to be 226 and after treatment Mean PBAC was decreased to 113 (p <0.0001).
When comparing the two groups, norethisterone caused a greater decrease in PBAC score, and this difference was statistically significant (p 0.0001). As the data gives the amount of blood loss in a cycle, based on the severity of DUB can be noted, and based on that the treatment plan can be decided by the physician.
Discussion
The term “dysfunctional uterine bleeding” (DUB) refers to any abnormal uterine bleeding, including modifications to the menstrual cycle, frequent and infrequent uterine bleeding, and alterations in the frequency or duration of menstrual loss. It most often refers to excessive regular menstrual bleeding or vital menorrhagia, though it can allude to any abnormal uterine bleeding. 1 DUB is a common gynecological ailment that is significant among the most upsetting to both the patient and the doctor. Although the exact origin of DUB is unknown, it is hypothesized that the hypothalamic-pituitary-ovarian axis is disrupted. 17. In a study by Deeksha Pandey, The third most frequent reason for the hysterectomy, after fibroid and prolapse, was DUB. Hysterectomy is also associated with intraoperative and postoperative complications. Rates of various complications with hysterectomy have been reported in the range from 0.5% to 43%18. Hysterectomy has recognised consequences like most major operations. Women who need surgery frequently do it in small hospitals with undertrained staff because of poverty, ignorance, and illiteracy in low-resource areas where they are disadvantaged, anaemic, and have less access to excellent treatment, increasing their risk of morbidity and mortality. The third most frequent reason for the hysterectomy, after fibroid and prolapse, was DUB. Menorrhagia and AUB should therefore have a successful non-surgical treatment, and surgery should only be performed as a last resort. You can utilize Norethisterone (NE) and Medroxyprogesterone (MPA), two potent medications, in the DUB. One type of female hormone is medroxyprogesterone (progestin). This drug is comparable to the progesterone our bodies naturally produce. This inhibits uterine enlargement in menopausal women taking oestrogen and cures painful, erratic, or missing menstrual cycles (another female hormone). It also functions as a contraceptive.The progestin drug norethisterone sometimes referred to as norethindrone, it cures secondary amenorrhea, uterine bleeding brought on by erroneous hormone levels, and endometriosis. The two drugs are given in different doses, duration, and frequencies, NE (5mg × 25 days ie; 2 stat, 1-1-1 × 3 days, 1-0-1 × 21 days) and MPA (10mg × 21 days, 1-0-1). This study’s findings are comparable to those of other research. In this study, DUB was more common in women over the age of 35 in both therapy groups (NE – 74.3% & MPA – 75%). According to research by Nair et al, Kumari et al, and Sinha et al, people between the ages of 40 and 50 had a high frequency of DUB. 19-21 As the mean volume of the uterus will change with aging, the mean volume of the uterus of women aged 18-35 years is 38.55+/-3.68cm, and in women with age >35 years is 24.02+/- ie; with the increase in age the mean volume of the uterus get decreased so the chance of DUB is more with aging, also with an increase in age- muscle, ligaments and other tissues of the uterus get prolapsed, as the pelvic pressure increases, it will increase the chance of opening of the vagina- it leads to abnormal bleeding. In young womens bleeding will be mainly due to birth control pills and pregnancy. Depending on the level of schooling About 41.1% of the patients in the NE group were graduates, followed by 10.2% of patients with just primary school education, 28.2% of patients with higher secondary education, and 20.5% of patients with high school education. In the MPA group, there were around 40.6% graduates, 21.8% higher secondary school graduates, 27.9% high school graduates, and 9.3% primary school graduates. The patient is given counseling based on his or her educational position ie; if a patient is illiterate then the counselling should be given in a very simple way mainly medical terms should be avoided and the consent form, questionnaires should be explained in their local languages and for literate patient it can be done in a professional manner. According to marital status In the NE group, married women made up 89.7% of patients, while single women made up 10.3% of patients. In the MPA group, married women made up 90.6% of the patients, while single women made up 9.4%. DUB is therefore more common among married women in both groups. According to a study by Khadim MT and colleagues, DUB is more common in married women (91.1%) and less common in unmarried women (8.9%). 22 In married women, stress, alterations in daily routine, changes in body weight (fast or major weight gain will have a very negative impact on uterine bleeding), and use of hormonal birth control pills are the main causes of DUB.
According to the body’s mass index (BMI), In the NE group, 56.4% of patients fell into the overweight (25-29.9) category, 30.7% of patients fell into the normal (18.5-24.9) category, 7.6% of patients fell into the obesity (>29.9%) category, and 5.1% of patients fell into the underweight (18.5 kg) category. In the MPA group, 50.1% of patients fell into the overweight (25-29.9) category, 28.1% of patients fell into the normal (18.5-24.9) category, 12.5% of patients fell into the underweight (18.5) category, and 9.3% of patients fell into the obesity (>29.9%) category, indicating that overweight is also a factor in DUB development. Obesity is the primary cause of DUB, according to investigations by Casablanca Y et al. and Nouri M et al. 23-24 Obese patients have a higher risk of DUB due to a delayed endometrial repair, oestrogen levels are elevated (adipose tissue stored in the abdomen and body convert fat-producing hormone to oestrogen); high BMI is also a risk factor for endometrial cancer and also the obese patients have the chance of producing Polycystic ovarian syndrome, it can also lead to DUB. Treatment with NE and MPA risen haemoglobin levels from 8.2g% to 10.6g% and 8.3g% to 10.2g%, respectively. Hemoglobin levels increased in both groups after treatment, as in this study. Similar studies were conducted by Kriplani et al and Komaram et al, and the mean haemoglobin risen from 10.6% to 11.2% and 9.2% to 10.5%, respectively. 25-26 In a normal menstrual cycle the blood loss is around 60ml but in DUB the loss of blood is more than 80ml, So the chances of decrease in haemoglobin level is much more, As the volume of blood rises by treating the DUB properly, the amount of bleeding get declined. In accordance with the sonographic findings, In the NE group, there were 9 patients (23%) with endometriosis, 8 patients (20.5%) with leiomyoma, 7 patients (17.9%) with polyp, 7 patients (17.9%) with ovulatory disorder, 5 patients (12.8%) with adenomyoma, and 2 patients (5.1%) with malignancy. In the MPA group, there were 10 patients (31.2%) with leiomyoma, 7 patients (21.8%) with endometriosis, 6 patients (18.7%) with ovulatory disorder, 5 patients (15.6%) with polyp, 3 patients (9.3%) with adenomyoma, and 1 patient (3.1%) with malignancyThe findings are consistent with those of Singh et al and Sinha et al, who found similar incidences in their research..27, 21 they are mainly structural and functional components .The higher incidence of patients was with endomteriosis and leiomyoma. The ultrasonographic findings are classified based on PALM (structural) –COIEN (non-structural) classification. In structural entities , mainly the outgrowths are seen in the uterus and in non-structural entities , mainly bleeding disorders , ovulatory dysfunctions are seen.30 In the study, PBAC scores lowered from 230 to 96 after treatment with NE, and PBAC scores lowered from 226 to 113 after treatment with MPA. As the PBAC score lowered means the decrease in usage of number of pads/tampons are noted, also the spotting and clotting will get disappeared and the heaviness of bleeding get decreased. Treatment with NE was discovered to be more beneficial than MPA in this study. Agarwal N et al and Shravage et al studies on the efficacy of Norethisterone and Medroxyprogesterone in DUB were similar to this study. 28-29
Conclusion
DUB (dysfunctional uterine bleeding) is a common gynecological issue. The majority of patients respond favorably to medical treatment. Norethisterone and Medroxyprogesterone are both effective in treating these cases, as made evident by a decrease in PBAC score, subjective upgrade, and an increase in hemoglobin level. DUB was more frequent in women over the age of 35, due to a rise in uterine mean volume. DUB is most common in women with a high BMI (25-29.9-overweight), and it is affected by delayed endometrial repair. However, Norethisterone has a much stronger effect. Thus, Norethisterone was discovered to be more effective than Medroxyprogesterone in lowering menstrual loss as the effect is evaluated by assessing the PBAC chart , the PBAC score were lowered more in NE patients when compared with MPA group. A significant development in the DUB management has been shown while using NE and MPA ie; the rate of hysterectomy has been decreased in large volume in both the rural and urban areas. Neither drug has any significant side effects or complications.
Acknowledgment
The authors would like to thank all staff members of the department of Obstetrics and Gynecology of Paalana Institute of Medical Sciences, Palakkad, Kerala for their kind support.
Conflicts of Interest
There are no conflicts of interest between the authors
Reference
- Yaaqoub NK. A comparative study between norethisterone progestogens and dydrogesterone in the treatment of dysfunctional uterine bleeding. Am Medical J. 2010; 1:23-6.
CrossRef - Betha K, Malavatu L, Talasani S. Distribution of causes of abnormal uterine bleeding using new FIGO classification system-PALM COEIN: a rural tertiary hospital based study. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2017; 6(8): 3523-7.
CrossRef - Lobo RA. Abnormal uterine bleeding: ovulatory and anovulatory dysfunctional uterine bleeding: management of acute and chronic excessive bleeding. In: Lentz GM, Lobo RA, Gershenson DM, et al, eds. Comprehensive Gynecology. Philadelphia: Mosby-Elsevier; 2012:805-814. (Textbook chapter)
CrossRef - Tibbles CD. Selected gynecologic disorders: abnormal uterine bleeding in the nonpregnant patient. In: Marx JA, Hockberger RS, Walls RM, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. Philadelphia, PA: Mosby-Elsevier; 2010: 1325-1332. (Textbook chapter)
CrossRef - Oehler MK, Rees MCP. Menorrhagia: an update. Acta Obstet Gynecol Scand. 2003;82(5):405-422.
CrossRef - Hashim HA, Alsherbini W, Bazeed M. Contraceptive vaginal ring treatment of heavy menstrual bleeding: a randomized controlled trial with norethisterone. Contraception. 2012 Mar 1; 85(3):246-52.
CrossRef - Vaidya r, vinayachandran s, devi s, prejisha b, lekshminath g, sreedharan s, jahrin p. Prevalence of Abnormal Uterine Bleeding and its Associated Risk Factors in Women of Perimenopausal Age Group-A Retrospective Study. Journal of Clinical & Diagnostic Research. 2022 Dec 1;16(12).
CrossRef - https://www.accessdata.fda.gov/drugsatfda_docs/label/2007/011839s071lbl.pdf
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/020527s065lbl.pdf
- Johansson ED, Johansen PB, Rasmussen SN: Medroxyprogesterone acetate pharmacokinetics following oral high-dose administration in humans: a bioavailability evaluation of a new MPA tablet formulation. Acta Pharmacol Toxicol (Copenh). 1986 May;58(5):311-7. doi: 10.1111/j.1600-0773.1986.tb00115.x.
CrossRef - Sierra-Ramirez JA, Lara-Ricalde R, Lujan M, Velazquez-Ramirez N, Godinez-Victoria M, Hernadez-Munguia IA, Padilla A, Garza-Flores J: Comparative pharmacokinetics and pharmacodynamics after subcutaneous and intramuscular administration of medroxyprogesterone acetate (25 mg) and estradiol cypionate (5 mg). Contraception. 2011 Dec;84(6):565-70. doi: 10.1016/j.contraception.2011.03.014. Epub 2011 May 11.
CrossRef - Sitruk-Ware R: Pharmacological profile of progestins. Maturitas. 2004 Apr 15;47(4):277-83
CrossRef - Gompel A: Progesterone, progestins and the endometrium in perimenopause and in menopausal hormone therapy. Climacteric. 2018 Aug;21(4):321-325. doi: 10.1080/13697137.2018.1446932. Epub 2018 Mar 27
CrossRef - Barra F, Scala C, Ferrero S: Current understanding on pharmacokinetics, clinical efficacy and safety of progestins for treating pain associated to endometriosis. Expert Opin Drug Metab Toxicol. 2018 Apr;14(4):399-415. doi: 10.1080/17425255.2018.1461840. Epub 2018 Apr 10.
CrossRef - Magnay JL, O’Brien S, Gerlinger C, Seitz C. Pictorial methods to assess heavy menstrual bleeding in research and clinical practice: a systematic literature review. BMC women’s health. 2020 Dec;20(1):1-5.
CrossRef - Godha Z, Mohsin Z, Hakim S, Wasim S. Comparative study of Ormeloxifene and Medroxyprogesterone acetate in abnormal uterine bleeding. The Journal of Obstetrics and Gynecology of India. 2016 Oct; 66(1):395-9.
CrossRef - Livingstone M, Fraser IS. Mechanisms of abnormal uterine bleeding. Hum Reprod Update 2002; 8:60-7.
CrossRef - Pandey D, Sehgal K, Saxena A, Hebbar S, Nambiar J, Bhat RG. An audit of indications, complications, and justification of hysterectomies at a teaching hospital in India. International journal of reproductive medicine. 2014 Jan 2;2014.
CrossRef - Nair R, Mallikarjuna M. Clinical profile of patients with abnormal uterine bleeding at a tertiary care hospital. Int J Reprod Contracept Obstet Gynecol. 2015; 4:1753-7.
CrossRef - Kumari A, Kumar R. Abnormal uterine bleeding in peri- menopausal age: An observational study. Indian J Obstet Gynecol Res. 2018; 5(4):539-43.
CrossRef - Sinha K, Gurung P, Sinha HH, Bhadani PP. Study on abnormal uterine bleeding among adult women in a tertiary care hospital in Bihar, India. Int J Reprod Contracept Obstet Gynecol. 2018; 7:3136-40.
CrossRef - Khadim MT, Zehra T, Ashraf HM. Morphological study of Pipelle biopsy specimens in cases of abnormal uterine bleeding. J Pak Med Assoc. 2015 Jul 1; 65(7):705-09.
- Nouri M, Tavakkolian A, Mousavi SR. Association of dysfunctional uterine bleeding with high body mass index and obesity as a main predisposing factor. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2014 Jan 1; 8(1):1-2.
CrossRef - Casablanca Y. Management of dysfunctional uterine bleeding. Obstet Gynecol Clin North Am 2008; 35(2):219–34.
CrossRef - Kriplani A, Kulshrestha V, Agarwal N. Efficacy and safety of ormeloxifene in management of menorrhagia: a pilot study. J Obstet Gynaecol Res. 2009; 35:746–52.
CrossRef - Komaram R, Palla J, Chintada GS. A study of ormeloxifene in the pharmacological management of dysfunctional uterine bleeding. J Clin Diagn Res. 2013; 7(11):2534–6.
- Singh P. Abnormal uterine bleeding-evaluation by endometrial aspiration. J Mid-life Health. 2018; 9:32- 5.
CrossRef - Agarwal N, Singh S, Singh S, Agarwal M, Manocha P. Comparative evaluation of the efficacy and safety of ormeloxifene and norethisterone in dysfunctional uterine bleeding. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2013 Jun 1; 2(2):194-9.
CrossRef - Jyotsna Sharvage, Mekhala D, et al. Ormeloxifene versus medroxyprogesterone acetate (MPA) in the treatment of dysfunctional uterine bleeding: a double blind randomized controlled trial. J South Asian Fed Obstet Gynaecol. 2011; 3(1):21–4.
CrossRef - Chodankar R, Critchley HO. Abnormal uterine bleeding (including PALM COEIN classification). Obstetrics, Gynaecology & Reproductive Medicine. 2019 Apr 1;29(4):98-104.
CrossRef

This work is licensed under a Creative Commons Attribution 4.0 International License.





