How to Cite | Publication History | PlumX Article Matrix
Bridging Biochemistry and Aging: A Journey Towards Prolonged Health span
Department of Pharmacy, Sumandeep Vidyapeeth Deemed to be University, Piparia, Waghodia, Vadodara, Gujarat, India.
Corresponding Author E-mail:neil.dop@sumandeepvidyapeethdu.edu.in
DOI : http://dx.doi.org/10.13005/bbra/3226
ABSTRACT: Aging involves intricate molecular, cellular and systemic changes over time. Biochemical research has illuminated mechanisms underlying age-related functional decline and revealed promising targets to extend healthspan. Mitochondrial dysfunction, telomere attrition, and impaired proteostasis contribute to aging. However, cellular senescence, marked by arrested proliferation and secretion of proinflammatory factors, has emerged as a central driver. Senolytics, drugs that selectively eliminate senescent cells, alleviate multiple age-related phenotypes in animal models. Stem cell exhaustion also impairs tissue homeostasis. Rejuvenating endogenous stem cell populations could help restore youthful regeneration. Epigenetic alterations lead to aberrant gene regulation, while inflammation and immunosenescence disrupt tissue function. Caloric restriction robustly extends lifespan in animals, but optimally translating this to humans remains challenging. Elucidating interactions between genetics, epigenetics, and lifestyle provides insights into precision interventions tailored to an individual’s aging profile. New technologies like epigenome editing may eventually reprogram aged cells into more youthful states. Metabolic engineering through pathways related to mitochondria, inflammation, and nutrition also shows promise. Realizing the potential of emerging strategies to prolong human healthspan demands collaborative, interdisciplinary efforts spanning from molecular discoveries to clinical implementations, guided by ethical frameworks for responsible translation. Innovative biogerontology research portends a future where healthspan is not constrained by the biological march of time but extended through science thoughtfully applied for the benefit of humankind.
KEYWORDS: Cellular senescence; Epigenetics; Mitochondrial dysfunction; Proteostasis; Stem cell exhaustion
Download this article as:| Copy the following to cite this article: Panchal N. B. Bridging Biochemistry and Aging: A Journey Towards Prolonged Health span. Biotech Res Asia 2024;21(1). |
| Copy the following to cite this URL: Panchal N. B. Bridging Biochemistry and Aging: A Journey Towards Prolonged Health span. Biotech Res Asia 2024;21(1). Available from: https://bit.ly/3VyzzFh |
Introduction
Aging is characterized by the gradual biological decline of cells, tissues, and organisms over time. Lifespan refers to the maximum number of years an organism can survive, while healthspan denotes the years of life spent in good health. As global life expectancy rises, the elderly population is expanding rapidly. This demographic shift comes with various socioeconomic challenges, as aging is the primary risk factor for many chronic diseases like cancer, diabetes, and neurodegenerative disorders1 Understanding the molecular underpinnings of aging is crucial to extend healthspan and develop interventions that delay or prevent age-related functional decline. Key molecular and cellular hallmarks of aging that represent promising targets include genomic instability, telomere attrition, epigenetic alterations, proteostasis, mitochondrial dysfunction, cellular senescence, stem cell exhaustion, and altered intercellular communication2.
Aging is a complex biological process involving multiple theories and mechanisms. The free radical theory postulates that oxidative damage from reactive oxygen species causes cumulative damage to cells and tissues over time3. Telomere shortening limits the replicative capacity of cells, eventually triggering senescence. Mitochondrial dysfunction and impaired quality control systems can also promote cellular aging. At the tissue level, altered intercellular communication and exhaustion of stem cell pools may contribute to loss of homeostasis and regenerative capacity4. Overall, these processes lead to genomic instability, epigenetic changes, loss of proteostasis, metabolic dysfunction, inflammation, and cellular senescence2.
This review will provide an in-depth exploration of the key molecular factors and biochemical pathways implicated in driving mammalian aging. Cellular senescence, oxidative stress, mitochondrial dysfunction, and declining genomic integrity appear to be particularly important processes based on extensive research in model organisms and human studies. Understanding these mechanisms at a molecular level may reveal promising targets for interventions to extend human health span. Lifestyle approaches like caloric restriction and pharmacological strategies to remove senescent cells or boost antioxidant defenses have already shown success in animal models. Translating these findings to humans remains an active area of geroscience research. Overall, illuminating the intricate biochemistry underlying aging will open new possibilities for promoting healthy longevity.
Theories of Aging
 |
Figure 1: Overview of Theories of Aging |
The free radical theory, first proposed in the 1950s5, holds that reactive oxygen species (ROS)-inflicted damage drives aging. Free radicals directly damage proteins, lipids, DNA, and other cellular components6. Moreover, impaired antioxidant defenses fail to adequately neutralize accumulating free radicals as organisms age. Initial support came from model organism studies demonstrating extended lifespan when antioxidant activity is genetically or pharmacologically boosted. However, clinical trials of general oral antioxidants in humans have not proven successful against aging biomarkers or age-related diseases7. While antioxidants may mitigate some oxidative damage, more targeted interventions may be needed to prevent free radical-induced functional decline.
The telomere shortening theory links aging to erosion of telomeres, protective nucleotide repeats at chromosome ends that promote genomic stability8. Telomeres progressively shorten with cell division due to the end replication problem, eventually triggering replicative senescence once critically short9. Accelerated telomere attrition associates with premature aging disorders like dyskeratosis congenita. Expressing telomerase, the enzyme that maintains telomere length, extends cellular and whole organism lifespan in mice10. However, telomerase mutations only explain some human progeroid syndromes11,12, indicating additional mechanisms substantially contribute to aging. Therapies to sustain telomere length may help delay certain facets of aging, but cannot fully reverse the complex cellular and systemic changes13,14.
Caloric restriction (CR) is one of the most robust interventions known to extend healthy lifespan across diverse species, including yeast, flies, worms, and rodents15,16. Restricting calories appears to trigger evolutionarily conserved cellular signaling pathways mediated by sirtuins, AMPK, and other regulators that enhance stress resistance and protein homeostasis17,18. However, implementing extreme long-term CR in humans is challenging. Alternate day fasting or pharmaceutical CR-mimetics are being investigated for their efficacy in improving human healthspan19,20. Data is still limited regarding their translation from animal models.
The mitochondrial theory posits accumulation of mitochondrial DNA (mtDNA) mutations progressively impairs oxidative phosphorylation, disrupting cellular energy homeostasis over time21. Gradual ATP decline, increased mitochondrial reactive oxygen species leakage, and abnormal mitochondrial dynamics are observed in aging22. Yet directly boosting mitochondrial biogenesis only modestly increases lifespan in animal models4, implying mitochondrial dysfunction alone cannot explain aging. Mitochondrial targeted therapies may be most effective when combined with interventions that address other age-related processes like cellular senescence23,24.
Cellular senescence entails essentially irreversible cell cycle arrest along with secretion of pro-inflammatory cytokines, proteases, and other factors that impair tissue function. Senescent cells accumulate in tissues with age and at sites of pathology. Removing them via senolytic drugs alleviates, prevents, or even reverses multiple age-related phenotypes and diseases in mice. This demonstrates causality between senescent cell burden and aging25. Senescent cell clearance is now considered a highly promising approach to enhance healthy lifespan. Ongoing clinical trials are beginning to assess senolytic therapies in humans26.
While no single theory fully explains the multifaceted biology of aging, elements of the free radical, telomere attrition, nutrient signaling, and mitochondrial theories likely combine to drive age-related functional decline2. But cellular senescence has gained prominence as a central mechanism due to the strength of genetic, pharmacological, and emerging clinical data25,27. Ongoing research continues to uncover how these processes interact across scales from molecules to cells to tissues to orchestrate aging’s progression. Combination therapies targeting senescent cells, oxidative damage, mitochondrial health, and other factors may prove most effective at prolonging human healthspan28.
Cellular Senescence and Aging
Cellular senescence entails essentially irreversible cell cycle arrest, rendering cells unable to proliferate even when stimulated. Senescence is triggered by telomere erosion, DNA damage, mitochondrial dysfunction, oncogene activation, and other stressors29. Once perceived as a tumor suppression mechanism, senescent cells accumulate in tissues with age and secrete inflammatory factors that impair tissue structure and function. This senescence-associated secretory phenotype (SASP) involves proteases, chemokines, and cytokines that can foster chronic inflammation30. Senescent cells promote the development of age-related pathologies including atherosclerosis, osteoarthritis, cancer, and metabolic dysfunction.25
Two major signaling pathways regulate senescence – p53/p21 responds to DNA damage while p16/Rb responds to stressors like oxidative damage31. While distinct, interconnections exist between them. Beyond halting proliferation, senescent cells secrete metalloproteinases that remodel extracellular matrix, disrupting tissue integrity32. Proinflammatory cytokines induce local inflammation33. Growth factors stimulate precancerous cell proliferation[34]. Vasoactive factors impair circulation. Through these effects, the SASP can profoundly alter tissue microenvironments.
Senescent cell burden escalates with natural aging and at sites of age-related pathology25. Mouse studies reveal removing p16-positive senescent cells via genetic, antibody, or senolytic approaches effectively alleviates multiple age-related disorders35. Senolytic compounds like navitoclax exploit the susceptibility of senescent cells to apoptosis. Eliminating senescent cells can enhance healthspan, physical function, and alleviate neurodegeneration in animal models36.
Several senolytic agents are now being assessed in early phase clinical trials for effects on human healthspan and age-related diseases. While translation continues, initial results demonstrate senescent cell reductions following treatment. Combining senolytics with lifestyle changes, NAD+ boosters, or mTOR inhibition may amplify benefits.
In the vast tapestry of aging, cellular senescence weaves an intricate narrative, transforming from a guardian to harbinger of age-related functional decline. The SASP broadcasts inflammatory signals that disrupt tissue equilibrium. Once-tolerant environments become landscapes of chronic inflammation as the immune system’s restorative efforts turn deleterious30.
Senolytics are emerging as compelling senescence-targeting therapies. By dismantling survival mechanisms of senescent cells and enabling their clearance, senolytics may mitigate SASP-associated inflammation and degeneration37. Animal studies reveal senolytics can delay, prevent, or even reverse diverse age-related diseases25. Clinical translation continues, guided by ethical imperatives of responsible and equitable translational research38.
While all dimensions of cellular senescence remain incompletely elucidated, its accumulation increasingly appears to be a principal conductor of tissue dysfunction, chronic inflammation, and other hallmarks of aging39. Targeted removal of senescent cells offers a promising therapeutic avenue to potentially restore more youthful tissue function and resilience. Further research into the nuanced biology of cellular senescence will uncover new possibilities for interventions that may help extend human healthspan40.
Telomere Shortening and Cellular Replication: The Elegant Dance of Cellular Integrity
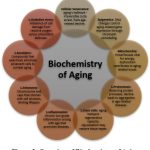 |
Figure 2: Overview of Biochemistry of Aging |
In the intricate choreography of cellular existence, a simple yet profound mechanism emerges as both a guardian and a harbinger of aging – the phenomenon of telomere shortening during cellular replication. This process, reminiscent of the fading resonance of a distant chime, encapsulates the very essence of cellular integrity. It delicately unveils the intricate interplay between rejuvenation and the inexorable flow of time41. Telomere attrition elucidates the profound connection between genomic stability, cellular replicative potential, and longevity42. As the sentinel caps dwindle with each cell division, so does the capacity for further proliferation until the onset of senescence. The integrity of the telomeric defense thus sets the rhythm of the cellular life cycle.
Telomeres, those protective caps nestled at the termini of chromosomes, are often likened to the aglets gracing the tips of shoelaces. Comprising repetitive DNA sequences, these sentinels are entrusted with preserving chromosomal stability during the process of cellular replication43. However, with each division, a portion of these protective caps is relinquished, yielding to the “end replication problem44.” This elegant mechanism safeguards the essential genetic blueprint within chromosomes, preventing unintended disruptions and mutations during the replication process45.
As cells undergo division, the gradual attrition of telomere length assumes the role of a biological hourglass, counting down the number of divisions a cell can undergo before crossing a critical threshold46. When telomeres reach this critical length, they signal a halt to cellular replication, ushering the cell into a state of senescence – an irreversible state of growth arrest47. This built-in mechanism serves as a vital defense against uncontrolled replication, a cornerstone of cancer prevention, ensuring that cells harboring potential mutations or damage do not perpetuate, thereby mitigating the risk of tumorigenesis48.
The nexus between telomere shortening and the aging process emerges as a double-edged sword. On one hand, the gradual erosion of telomeres forms a protective barricade against the unfettered growth characteristic of cancer, a fundamental aspect of preserving cellular integrity49. Conversely, this very process contributes to the incremental wane observed in functional capabilities as the years advance. As cells undergo senescence due to critically shortened telomeres, the rejuvenation of vital tissues is compromised, resulting in frailty and a heightened susceptibility to age-associated ailments50.
In certain instances, genetic predisposition or external factors can accelerate telomere attrition, culminating in premature aging disorders. An exemplar is Dyskeratosis Congenita, a condition where mutations in genes responsible for telomere maintenance provoke early-onset aging symptoms51,52. This poignant link between accelerated telomere diminution and premature aging underscores the pivotal role played by telomeres in sustaining cellular well-being, while underscoring the intricate equilibrium they maintain in orchestrating the symphony of the aging process53. Dyskeratosis congenita resulting from defective telomere maintenance illuminates the connection between short telomeres and tissue atrophy, demonstrating how accelerated erosion can mimic physiological aging. Telomere biology is thus intricately woven with human healthspan.54,55
As the narrative of telomere shortening unfolds, a ray of optimism emerges in the form of telomerase – an enzyme endowed with the capacity to elongate telomeres. While primarily active during early developmental stages and within certain stem cell populations, telomerase’s activity wanes in most somatic cells with advancing age. Reactivating this enzyme presents the prospect of cellular rejuvenation, as underscored by studies revealing extended cellular lifespan through telomerase expression56.
Yet, this promise of telomerase reactivation navigates through a labyrinth of intricacies. While it holds the potential to enhance cellular vitality, excessive expression can tip the equilibrium toward unchecked cellular proliferation, potentially fostering the development of cancer57. Striking the delicate balance between harnessing the therapeutic potential of telomerase and the looming risk of tumorigenesis becomes a high-stakes endeavor in the quest to elongate cellular healthspan.
In summation, the journey of telomere shortening during cellular replication unfolds as a tale of dual roles – functioning as guardians against cancer while simultaneously heralding the advent of aging. These vigilant sentinels, perched at the chromosome’s ends, stand as staunch defenders of genomic stability. Their gradual attrition, while shielding against cancerous proliferation, also contributes to the mosaic of aging. Unveiling the intricate equilibrium between telomeres, cellular replication, and rejuvenation offers a pathway to extend healthspan. The elusive promise of telomerase reactivation, embodying both promise and peril, beckons us to navigate the complex terrain of cellular vitality and the intricate dance with tumorigenesis. As we unlock the enigma embedded within our chromosomal tapestry, the symphony of telomeres resonates as a poignant portrayal of the profound interplay between life, the passage of time, and the tenacity of cellular integrity.
Epigenetic Changes and Aging: Unraveling the Molecular Tapestry
In the intricate realm of cellular biology, the phenomenon of aging is etched not only in the genetic code but also in the epigenetic landscape – a dynamic and intricate molecular tapestry that orchestrates gene expression patterns. Epigenetic changes, delicate alterations to the way genes are regulated without altering the underlying DNA sequence, emerge as crucial actors in the symphony of aging. This exploration delves into the intricate world of epigenetic modifications and their profound impact on the aging process[2]. The aging epigenome provides a pivotal molecular interface through which genetic and environmental cues shape gene expression changes over time. Elucidating the epigenetics of aging promises foundational insights into functional decline while revealing possibilities for interventions to modulate the epigenomic equilibrium58,59.
Epigenetics, often likened to the conductors of a hidden orchestra, governs gene expression patterns without altering the genetic code itself. The DNA sequence remains constant, but the epigenetic marks, akin to musical notes, dictate which genes are turned on or off in response to environmental cues and developmental needs. These marks include DNA methylation, histone modifications, and non-coding RNAs, collectively weaving the intricate tale of cellular identity and function60.
As time unfurls, the epigenetic landscape undergoes gradual changes. The once precise symphony of gene expression becomes a bit more discordant. This phenomenon, termed epigenetic drift, contributes to the progressive alterations observed with aging61. Epigenetic changes impact not only individual cells but can have profound effects on tissues, contributing to age-related functional decline and increased vulnerability to diseases58,59].
DNA methylation, the attachment of methyl groups to specific DNA sequences, is a hallmark of epigenetic regulation. In aging, the landscape of DNA methylation undergoes alterations. Certain genes may become hypermethylated, effectively silencing them, while others experience hypomethylation, potentially leading to their inappropriate activation. These changes can perturb finely tuned processes, contributing to cellular dysfunction and tissue decline62.
Histones, proteins around which DNA is wound, undergo a symphony of modifications that shape chromatin structure and gene accessibility. With aging, these histone modifications experience alterations, influencing the accessibility of genes to the cellular machinery63,64. The tightening or loosening of chromatin can lead to the repression or activation of critical genes, influencing cellular function and contributing to the aging phenotype65.
Non-coding RNAs, once dismissed as genetic “noise,” have emerged as potent regulators of gene expression. MicroRNAs and long non-coding RNAs orchestrate a delicate ballet, influencing the translation of genetic information into functional proteins66–68. With age, the expression patterns of these non-coding RNAs shift, impacting processes such as inflammation, tissue regeneration, and cellular stress responses69.
The concept of biological age, distinct from chronological age, has gained prominence with the emergence of epigenetic clocks. These clocks harness the predictive power of epigenetic changes to estimate an individual’s age, offering insights into their overall health and vulnerability to age-related diseases70. The epigenetic clock unravels the intricate link between the ticking of time and the molecular signatures imprinted within our cells60.
The tantalizing prospect of reversing epigenetic changes, akin to rewinding the aging clock, has sparked scientific curiosity. Experimental interventions, such as reprogramming cells to a more youthful state71 or utilizing specific molecules to restore epigenetic patterns72, hint at the potential to rejuvenate aging tissues73. However, these endeavors tread cautiously, navigating the intricate balance between cellular rejuvenation and the risk of unintended consequences.
In the grand tapestry of aging, epigenetic changes emerge as the subtle yet powerful weavers, intricately altering the genetic score without changing the notes74. These modifications influence cellular function, tissue vitality, and the vulnerability to age-related ailments. The symphony of DNA methylation, histone modifications, and non-coding RNAs shapes the story of aging, their dynamic interplay painting a canvas of cellular vitality and decline2,75,76.
As the scientific exploration of epigenetics deepens, a better understanding of these molecular nuances offers promise for interventions that might extend health span and mitigate age-related maladies. The journey into the world of epigenetic changes reminds us that while the passage of time is inevitable, the orchestration of cellular vitality remains an intricate dance between our genetic code and the epigenetic conductors that shape its expression.
Proteostasis and Aging: Balancing the Cellular Ledger
In the intricate landscape of cellular biology, where function emerges from molecular choreography, the equilibrium between protein production and degradation holds profound sway. This intricate balance, known as proteostasis, orchestrates the lifecycle of proteins, ensuring their timely creation, correct folding, and eventual removal. As the symphony of aging unfolds, proteostasis emerges as a central player, its harmonious rhythm disrupted by time’s inexorable march77. This exploration delves into the intricacies of proteostasis and its pivotal role in the aging narrative.
Proteins, the workhorses of cellular function, must maintain their intricate three-dimensional structures to execute their roles effectively. Proteostasis, often compared to an accounting ledger, entails a meticulous balance between protein synthesis, folding, and clearance78. When this equilibrium is perturbed, the cellular milieu becomes vulnerable to the accumulation of misfolded or damaged proteins, fostering the genesis of age-related maladies79,80.
Within the bustling cellular arena, molecular chaperones assume the roles of vigilant architects, overseeing the proper folding of nascent proteins. These chaperones, akin to skilled craftsmen, guide proteins along intricate pathways, ensuring they adopt their functional conformations81. With advancing age, the chaperone machinery encounters challenges, occasionally leading to the accumulation of misfolded proteins – a hallmark of aging cells82.
Equally crucial to proteostasis is the removal of proteins that have outlived their utility or adopted aberrant structures. The cellular machinery responsible for this task includes proteasomes and lysosomes, akin to recycling centers that dismantle proteins into their constituent parts83. With aging, the efficiency of these degradation pathways can wane, potentially resulting in the accumulation of toxic protein aggregates84,85.
At the intersection of proteostasis and cellular vitality lies autophagy – a dynamic process akin to a cellular cleanup crew. Autophagy engulfs damaged organelles and proteins, ferrying them to lysosomes for degradation and recycling. This process safeguards cellular health, preventing the accumulation of molecular clutter. However, with advancing age, autophagy’s efficiency can falter, contributing to cellular dysfunction and the emergence of age-related disorders86.
The intimate connection between proteostasis and neurodegenerative diseases paints a compelling portrait of their interplay. Disorders like Alzheimer’s, Parkinson’s, and Huntington’s are characterized by the accumulation of misfolded proteins within neurons. The breakdown of proteostasis mechanisms in these contexts serves as a potent contributor to disease progression, highlighting the intimate ties between proteostasis and the aging-associated decline in neuronal function87,88.
Oxidative stress, a consequence of an imbalance between the production of reactive oxygen species and the cellular machinery’s antioxidant defenses, casts its disruptive shadow upon proteostasis. Oxidative stress can damage proteins, perturb their folding, and impair the machinery responsible for their clearance89. As oxidative stress accumulates with age, its influence on proteostasis can foster the emergence of age-related ailments90.
The pursuit of interventions that sustain proteostasis and mitigate age-related maladies stands as a beacon of hope. Caloric restriction, which extends lifespan in model organisms, has been linked to enhanced proteostasis91. Pharmacological compounds that bolster chaperone activity or activate autophagy pathways hold promise for maintaining cellular vitality. Yet, these interventions navigate a complex landscape, requiring meticulous exploration to balance potential benefits with potential risks92.
Proteostasis, the intricate dance that sustains protein balance within cells, emerges as a protagonist in the aging narrative. Its harmonious rhythm safeguards cellular health, while its disruption serves as a harbinger of age-related dysfunction78. The symphony of proteostasis, with its molecular chaperones, recycling centers, and cellular cleanup crews, paints a canvas of cellular vitality and vulnerability77.
As we peer into the complexities of proteostasis, a better understanding emerges of its intimate connections with aging and age-related diseases93. The pursuit of interventions that preserve proteostasis offers a pathway to extending healthspan and mitigating the burdens of aging92. Yet, the proteostasis paradox remains, reminding us that while we seek to decipher its nuances, the symphony of cellular function continues to play out, an intricate interplay between balance and imbalance, resilience and vulnerability.
Inflammation and Immunosenescence: Navigating the Aging Immune Landscape
Inflammaging refers to the characteristic low-grade, chronic, systemic inflammation that emerges even in aged individuals lacking overt infection. In contrast to acute inflammation that resolves upon neutralizing inciting threats, inflammaging persists subclinically yet primes hyperactivation of inflammatory responses. This smoldering inflammation underlies the mild proinflammatory state frequently observed in the elderly94,95.
A constellation of factors kindles the subtle flames of inflammaging. Immunosenescence, the composite age-related alterations in immune cell populations and functionality, propagates dysregulated inflammatory responses. Thymic involution markedly reduces output of naïve T cells. Hematopoietic stem cell renewal capacity dwindles. Highly differentiated CD28- immunosenescent T cells accumulate, exhibiting telomere erosion, T cell receptor repertoire narrowing, and impaired proliferative potential. The decline in naïve:memory T cell ratios impedes adaptive immunity95,96.
Cellular senescence and associated secretory phenotype (SASP) drive sterilizing inflammation. The SASP entails secretion of proinflammatory cytokines, chemokines, growth factors, and matrix-remodeling proteases. Apoptotic cell debris also activates inflammasomes97,98.
Age-related physiological changes further kindle inflammatory fires. Adipose tissue accrual alters release of pro- and anti-inflammatory adipokines. Gut epithelial barrier disruption and microbiome dysbiosis increase systemic exposure to microbe-associated molecular patterns. Mitochondrial dysfunction elevates reactive oxygen species. Impaired autophagic clearance of damaged cellular components incites inflammasomes. Accumulation of advanced glycation end-products activates inflammatory signaling cascades99,100.
Unresolved inflammaging creates vulnerability to cytokine storm-mediated complications in infection and sustains pathologic inflammation underlying chronic diseases of aging including atherosclerosis, cancers, osteoporosis, and neurodegeneration. Developing targeted immunomodulatory interventions to selectively dampen detrimental age-related inflammation while preserving protective immune responses remains an active area of research.
Orchestrating the Rejuvenation of Aging Immunity
Immunosenescence and inflammaging are intricately intertwined. Chronic inflammation erodes immune homeostasis, causing paradoxical hyper-reactivity yet diminished effectiveness. The gradual unfurling of immunosenescence impacts various immune cell lineages. Composition and functionality of T cells, B cells, and innate immune cells are all affected101,94.
T cell immunosenescence is multifactorial. Thymic involution, chronic antigenic load, and inflammaging all contribute. Naïve T cell output wanes. Highly differentiated effector T cells accumulate. T cell receptor repertoire diversity narrows. CD28 expression is lost, compromising costimulation. Telomeres shorten, eventually inducing senescence. Immunosenescent T cells are prone to exhaustion, losing robust functionality96,102,103.
Reversing immunosenescence and restoring youthful immune function remains extremely challenging. Strategies range from revitalizing exhausted T cells to eliminating proinflammatory senescent cells to microbiome modulation104. However, calibrating the nuanced dynamics of inflammation and immunity in aging requires an intricate systems-level understanding105,106. Further research into mechanisms governing this delicate dance may reveal possibilities for enhancing protective immunity while mitigating detrimental inflammation across the lifespan.
Caloric Restriction and Sirtuins
Caloric restriction (CR), involving reduced calorie intake without malnutrition, has emerged as one of the most robust interventions known to extend healthy lifespan from yeast to mammals. CR triggers highly conserved cellular signalling pathways that reshape transcriptomes, proteomes, and metabolomes towards more youthful profiles. This metabolic remodelling enhances genomic and proteostatic integrity, mitochondrial function, autophagy, and metabolic health. Even short-term CR confers benefits, suggesting induction of longevity programs rather than merely slowing damage accumulation. However, implementing severe chronic CR in humans presents numerous challenges. This has intensified interest in developing caloric restriction mimetics (CRMs)107,108–110 – compounds that can replicate CR’s salutary effects by targeting key molecular mediators.
Sirtuins, a family of NAD+-dependent protein deacylases, have attracted great interest as prospective CR-responsive longevity factors. SIRT1 activates PGC-1α to promote mitochondrial biogenesis and antioxidant defenses while suppressing inflammation via NF-kB. SIRT3 enhances mitochondrial function and fat oxidation. SIRT6 maintains genomic stability. By increasing NAD+ levels, CR is believed to activate sirtuins and orchestrate adaptive stress responses. Experimental overexpression of specific sirtuins can extend lifespan in model organisms. However, while boosting sirtuin activity with NAD+ precursors shows potential, it has limitations in fully replicating CR’s multifactorial benefits111,112.
The energy sensor AMPK is also a key transducer of CR. By increasing AMP:ATP and ADP:ATP ratios, CR triggers AMPK phosphorylation to stimulate catabolic processes like autophagy and inhibit anabolic pathways. Metformin and other AMPK activators mimic certain CR responses but can also stimulate counterproductive negative feedback loops that attenuate benefits98,113,114.
Although sirtuins, AMPK, and additional regulators play important roles, CR likely elicits its pleiotropic effects through integrated molecular networks rather than isolated pathways. CR’s metabolic symphony fine-tunes mitochondrial efficiency, reduces damaging reactive oxygen species, and stimulates autophagic clearance of cellular debris. By quelling oxidative stress and inflammation, CR enhances cellular resilience against age-related diseases2,115. Interventions that comprehensively realign multiple hallmarks of aging hold promise as CR mimetics.
While CR shows remarkable lifespan extension in diverse animal models, translating such profound effects to humans has complexities. Beyond difficulties with compliance and nutritional adequacy, the optimal duration, timing, and regimens of CR for humans remain unclear. CR likely intersects with additional longevity pathways involving mTOR, insulin/IGF-1, AMPK, sirtuins, and more. Combining CR with drugs targeting these interconnected networks may therefore have synergistic benefits for prolonging human healthspan. However, the intricacies of how CR interfaces with the multifaceted biology of aging remain incompletely understood116,117. Further research into conserved adaptive mechanisms promises insights into targeted CR mimetics that may confer benefits without extreme dietary restriction.
Genetics, Epigenetics and Aging
The intricate biological chronicle of aging involves a complex interplay between genetic and epigenetic factors operating across multiple scales. Our unique DNA sequence comprises a genetic blueprint that profoundly influences aging traits and susceptibility to age-related diseases118. Both single nucleotide polymorphisms and mutations in specific genes can modulate the pace of aging by affecting protein structure and function119. However, epigenetic alterations that dynamically regulate gene expression without changing DNA sequence also accumulate over time and critically shape the aging process74.
Telomeres, protective caps composed of repetitive DNA sequences and specialized proteins at chromosome ends, play a vital role in cellular aging. Telomeres progressively shorten with each round of cell division due to the end replication problem, until critically short or damaged telomeres trigger replicative senescence45. Accelerated telomere attrition is associated with premature aging disorders like dyskeratosis congenita120. The enzyme telomerase can preserve telomere length by adding telomeric repeats, and extending telomerase expression promotes longevity in mice121. This underscores the importance of telomere integrity and length maintenance in sustaining cell proliferative capacity across the lifespan.
In addition to telomere erosion, diverse forms of genomic instability accumulate with age, including somatic mutations in mitochondrial DNA which encode components of the electron transport chain122,123. Gradual decline in the efficiency of DNA repair mechanisms that address DNA lesions, double strand breaks, base mismatches and other insults allows genomic damage to persist124. Unresolved errors lead to accumulation of deleterious mutations. Failure to adequately sense and resolve these persistent threats to overall genome integrity promotes cellular dysfunction on many levels.
Epigenetic alterations including DNA methylation, post-translational histone modifications, and chromatin remodelling dynamically regulate gene expression over time, independent of changes in DNA sequence. Gradual epigenetic drift leads to aberrant gene silencing or activation events that can profoundly disrupt cellular identity and function125,60. Changes in DNA methylation patterns affect expression of genes involved in critical processes like inflammation, stress response, and tissue regeneration[126]. Experimental interventions that reset a subset of age-related epigenetic marks have shown promising effects in restoring more youthful gene expression profiles and phenotypes126,127.
Lifestyle factors like diet, exercise and stress also influence the epigenome through complex gene-environment interactions. Caloric restriction, for example, can alter DNA methylation of genes associated with longevity and health span128,129. This hints at potential for epigenetic reprogramming via modulating external and internal cues to beneficially shape the aging trajectory130,131. However, directly editing the human epigenome as an anti-aging intervention remains an ongoing challenge rife with technical limitations and ethical uncertainties.
Genetic predispositions certainly shape an individual’s susceptibility to specific age-related diseases132,133, while accumulating epigenetic shifts alter gene regulatory patterns that sculpt broader aging traits134,75. Furthermore, genetic variations can tug on epigenetic pathways themselves135,136. This reveals how personalized interventions may eventually be designed to target both genetic risks and epigenetic dysfunction in an integrated, holistic manner. However, safely and effectively modulating the intricacies of the aging epigenome in humans is an enormously complex undertaking that remains on the frontier of aging research60.
In summary, genetics and epigenetics are deeply intertwined in regulating aging across scales from molecules to cells to tissues. Continued elucidation of their delicate molecular dance promises foundational insights into interventions that may ameliorate age-related functional decline at its biomolecular source, by supporting genome stability and optimizing epigenetic regulation. However, given the formidable ethical challenges and potential for unintended consequences, deftly translating emerging genetic and epigenetic insights into clinically viable human longevity therapies warrants ample caution along with hope.
Emerging Therapies and Stem Cell Rejuvenation for Extending Healthspan
 |
Figure 3: Emerging Therapies for Aging |
As aging research continues to illuminate the intricate biological processes involved, promising therapeutic approaches are rising on the horizon that may profoundly expand human healthspan. Cellular senescence has emerged as a principal aging mechanism, and senotherapeutics that selectively eliminate senescent cells represent a compelling vanguard anti-aging strategy137,138. Cellular senescence entails essentially irreversible cell cycle arrest along with secretion of proinflammatory, tissue-damaging factors collectively known as the senescence-associated secretory phenotype (SASP)139,140. Senescent cells accumulate in tissues with advancing age and at sites of pathology141,142. By alleviating the SASP, senolytic compounds may delay, prevent, or even reverse diverse age-related diseases. Excitingly, the first clinical trials are currently underway to evaluate the safety and efficacy of senolytic agents in humans143.
In parallel, strategies to rejuvenate exhausted adult stem cell populations across diverse tissues also hold great promise for re-establishing more youthful tissue regenerative capacity144,145. Stem cells serve as central pillars supporting homeostasis and repair throughout the lifespan. Their capacity for self-renewal and differentiation enables replacement of mature cells lost to turnover or damage. However, endogenous stem cells exhibit functional decline with advancing age in many organs, including hematopoietic, muscle satellite, neural, and other stem cell pools146,147. Changes underlying stem cell exhaustion include skewing of differentiation potential, telomere erosion, metabolic dysregulation, and impaired DNA repair148,149. Understanding the intricacies of age-related stem cell decline at a molecular level may inform genetic, pharmacological, or environmental interventions to reverse exhaustion and restore youthful tissue regenerative potential150,151. The prospect of rejuvenating aged stem cells offers renewed hope for strengthening, cognition, and resilience throughout the human lifespan.
In addition to senotherapeutics and stem cell rejuvenation, targeting the epigenome has attracted intense interest for its potential to recalibrate age-related gene expression changes that drive functional deterioration. The epigenome encompasses chromatin modifications, including DNA methylation, histone variants, and non-coding RNAs, that dynamically regulate gene expression independent of DNA sequence. Gradual epigenetic drift over decades leads to aberrant silencing or activation of genes that disrupt cellular identity and function. While still in its infancy, the burgeoning field of epigenetic editing holds promise as a means to reverse deleterious epigenetic marks and potentially rejuvenate aged cells and tissues. However, considerable technological hurdles remain in delivering epigenome editing complexes with sufficient safety, efficacy, and precision to realize clinical benefits.
Revealing the enigmas of aging hinges on unraveling the mysteries within mitochondria, the cellular powerhouses. Elevating mitochondrial function presents an avenue to alleviate the aging’s toll. Precision medicine, under the counsel of personalized genomic revelations, introduces an extra facet to the pursuit of extended health span. Conjointly, these methods propose a customized approach for every individual. As we delve deeper into the intricate interplay of mitochondria and genetics, the future landscape of aging adopts a personalized and revitalized complexion152–154. Furthermore, combination therapies that simultaneously target multiple hallmarks of aging may achieve synergistic benefits compared to isolated interventions2. However, optimizing combinatorial regimens requires a systems-level perspective and far more research elucidating complex biological interactions between therapies111. Ensuring safety and efficacy remains paramount as progressive lifespan-extending technologies advance through the translational pipeline116.
Thoughtful ethical frameworks must guide responsible translation as these disruptive technologies proceed from proof-of-concept to human trials. While myriad challenges exist, emerging senotherapeutics, stem cell rejuvenation, epigenome editing, and related interventions harbor truly transformative potential to prolong health span through innovative, collaborative biomedical research155. Capitalizing on synergies between approaches targeting molecular, cellular, and tissue processes offers an integrated path to combating aging’s complex biology and extending human vitality153.
Future Directions
Navigating the Uncharted Waters: Shaping the Future of Biochemistry and Aging
 |
Figure 4: Future prospects of Aging |
The confluence of biochemistry and aging is a journey of uncharted waters, with every new discovery offering a glimpse of the potential to extend human health span. The future lies in personalized precision interventions that consider the intricate interplay of genetics, epigenetics, and lifestyle factors156. The era of precision medicine beckons, and at its core lie biomarkers with the power to unveil the secrets of aging and disease susceptibility. These molecular signposts illuminate the path to personalized interventions that transcend one-size-fits-all solutions. The promise is profound: a bespoke approach that optimizes health span extension for each individual. As biomarkers continue to unravel the intricacies of aging, the future of tailored interventions shines brighter than ever157.
In the realm of emerging biochemistry frontiers, epigenetic engineering stands as a promising beacon. This burgeoning field offers a tantalizing promise – the ability to breathe new life into cellular functions. By deftly manipulating DNA methylation, shaping histone marks, and orchestrating non-coding RNA expression, epigenetic engineers envision a future where age-related cellular decline is reversed, ushering in a new era of health and vitality 158. As researchers unravel the complexities of epigenetic modifications, they pave the way for interventions that could potentially reverse age-related changes and restore cellular youthfulness159. Despite challenges, the power of epigenetic editing to address aging at the molecular level offers a transformative pathway to explore160.
The intersection of biochemistry and aging spotlights metabolism as a pivotal nexus with the power to slow down the aging clock. Within this domain, innovative strategies such as caloric restriction mimetics and agents that fine-tune energy production pathways hold the promise to combat oxidative stress, boost mitochondrial vitality, and rejuvenate cellular function. These interventions are like keys that unlock the potential for a longer, healthier life161. The intricate dance between metabolism and aging unveils novel strategies, but their exploration requires careful navigation of the intricate biochemical landscape.
Cellular senescence, once viewed as a singular concept in aging, has evolved into a nuanced understanding of its multifaceted effects on various tissues and diseases. We now recognize that senescence is not a uniform process but rather a spectrum of cellular states, impacting health in complex ways. This deeper comprehension enables the development of targeted interventions that selectively address the harmful aspects of senescence while preserving its potential benefits for tissue repair and regeneration162. Innovative senolytic compounds offer the prospect of selectively eliminating detrimental senescent cells while preserving beneficial aspects37. This precision targeting addresses age-related ailments with heightened accuracy, marking a significant step towards managing the impact of senescence on health span.
Interdisciplinary collaborations underscore the future trajectory of biochemistry and aging163. Geneticists, bioinformaticians, clinicians, and biochemists converge to unravel the molecular intricacies of aging, bridging the gap between scientific revelations and clinical applications164. This collaborative synergy catalyzes the translation of newfound insights into tangible interventions, transforming the landscape of healthspan extension.
In this exploration, ethical considerations accompany scientific advancement. The prospect of prolonged healthspan raises questions about resource allocation, societal structures, and the essence of existence. Crafting ethical frameworks to responsibly guide the application of emerging therapies becomes crucial. Striking a balance between the aspiration for prolonged vitality and the preservation of human dignity and quality of life remains paramount as we chart the unknown territories of biochemistry and aging[165].
Charting the Unknown: Pioneering the Age of Vitality
The evolving intersection of biochemistry and aging unveils a landscape brimming with potential. From personalized precision interventions to the intricate craft of epigenetic manipulation, the reengineering of metabolic pathways, and the artful targeting of senescence, the future is painted with vibrant promise. These innovative approaches hold the key to unlocking the secrets of aging, offering the potential for extended healthspan and a higher quality of life.[156] Guided by interdisciplinary collaborations and fortified by ethical considerations, the road ahead leads us to a realm where health span is not just prolonged but flourishes with vibrancy and resilience[166]. As the horizons of knowledge expand, the future of biochemistry and aging beckons – a canvas illuminated by the radiance of renewed vitality, stretching beyond the boundaries of yesterday’s imaginings
Conclusion
The intricate interplay between biochemistry and aging has unveiled a symphony of discoveries promising to reshape human healthspan’s trajectory. Diverse biological terrains shape aging’s progression, from mitochondrial dynamics to cellular senescence’s intricate choreography. Epigenetic patterns, proteostasis, inflammatory cascades, and caloric restriction’s nuanced influence converge in aging’s multifaceted narrative. Stem cell exhaustion underscores the need to rejuvenate regenerative capacity. Precision interventions tailored to an individual’s aging profile provide a path towards personalized longevity extension.
Propelling this future, interdisciplinary collaborations between science and the humanities offer immense potential, guided by ethical compasses. The fusion of biochemistry and aging thus paints a hopeful canvas, revealing horizons where vitality and resilience endure, unconstrained by the march of time. In this captivating tale, creativity and discernment come together, illuminating a future where aging is not typified by decline, but by the fulfillment of our most vibrant potential.
As the intricate dance between biochemistry and aging continues, emerging therapies harbor unprecedented possibilities to prolong healthspan and ameliorate the burdens of aging’s unfavorable finale. However, thoughtfully charting the course ahead requires embracing the complexity, calibrating potential with judicious optimism. While challenges remain, the accelerating pace of discovery gifts humanity with new levers to shape biology’s profound chronicles. If guided by collaborative wisdom, these tools may shift aging’s trajectory toward a destiny unbounded by the accustomed denouement of time. By unveiling the nuanced mechanisms sculpting our vital years, biochemistry offers fresh hope of illuminating the years ahead with enduring strength, creativity, and purpose.
Acknowledgement
I express my profound appreciation to Mr. Biren S. Panchal for the invaluable guidance and unwavering support throughout this research.
Conflicts of Interest
This research and its findings are driven purely by scientific merit and unwavering integrity, with no competing interests influencing our work.
Funding Sources
The author has independently prepared this paper for publication, drawing from their individual research and dedication.
Author Contributions
The author of this paper has adhered to the guidelines of the International Committee of Medical Journal Editors (ICMJE), made substantial contributions to the study, and have collectively endorsed the final manuscript for submission and publication.
Ethical Approvals
Given that this study did not involve animals or humans, no ethical clearance was required.
Data Availability
All data generated and analyzed for this study have been comprehensively documented within the research article.
References
- Niccoli T, Partridge L. Ageing as a risk factor for disease. Curr Biol [Internet] 2012 [cited 2023 Aug 27];22(17). Available from: https://pubmed.ncbi.nlm.nih.gov/22975005/
- López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell [Internet] 2013 [cited 2023 Aug 27];153(6):1194. Available from: https://pubmed.ncbi.nlm.nih.gov/23746838/
- Harman D. Aging: A Theory Based on Free Radical and Radiation Chemistry. Sci Aging Knowl Environ [Internet] 2002 [cited 2023 Aug 27];2002(37). Available from: https://www.science.org/doi/10.1126/sageke.2002.37.cp14
- Sharpless NE, DePinho RA. How stem cells age and why this makes us grow old. Nat Rev Mol Cell Biol [Internet] 2007 [cited 2023 Aug 27];8(9):703–13. Available from: https://pubmed.ncbi.nlm.nih.gov/17717515/
- Harman D. Aging: A Theory Based on Free Radical and Radiation Chemistry. Sci Aging Knowl Environ [Internet] 2002 [cited 2023 Aug 29];2002(37). Available from: https://www.science.org/doi/10.1126/sageke.2002.37.cp14
- Milisav I, Ribarič S, Poljsak B. Antioxidant Vitamins and Ageing. Subcell Biochem [Internet] 2018 [cited 2023 Aug 29];90:1–23. Available from: https://pubmed.ncbi.nlm.nih.gov/30779004/
- Bjelakovic G, Nikolova D, Gluud LL, Simonetti RG, Gluud C. Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases. Cochrane database Syst Rev [Internet] 2012 [cited 2023 Aug 29];2012(3). Available from: https://pubmed.ncbi.nlm.nih.gov/22419320/
- Jiang H, Ju Z, Rudolph KL. Telomere shortening and ageing. Z Gerontol Geriatr [Internet] 2007 [cited 2023 Aug 29];40(5):314–24. Available from: https://pubmed.ncbi.nlm.nih.gov/17943234/
- Martin H, Doumic M, Teixeira MT, Xu Z. Telomere shortening causes distinct cell division regimes during replicative senescence in Saccharomyces cerevisiae. Cell Biosci [Internet] 2021 [cited 2023 Aug 29];11(1):1–10. Available from: https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-021-00693-3
- Rossiello F, Jurk D, Passos JF, d’Adda di Fagagna F. Telomere dysfunction in ageing and age-related diseases. Nat Cell Biol 2022 242 [Internet] 2022 [cited 2023 Aug 29];24(2):135–47. Available from: https://www.nature.com/articles/s41556-022-00842-x
- Revy P, Kannengiesser C, Bertuch AA. Genetics of human telomere biology disorders. Nat Rev Genet 2022 242 [Internet] 2022 [cited 2023 Aug 29];24(2):86–108. Available from: https://www.nature.com/articles/s41576-022-00527-z
- Kam MLW, Nguyen TTT, Ngeow JYY. Telomere biology disorders. npj Genomic Med 2021 61 [Internet] 2021 [cited 2023 Aug 29];6(1):1–13. Available from: https://www.nature.com/articles/s41525-021-00198-5
- Mather KA, Jorm AF, Parslow RA, Christensen H. Is telomere length a biomarker of aging? A review. J Gerontol A Biol Sci Med Sci [Internet] 2011 [cited 2023 Aug 29];66(2):202–13. Available from: https://pubmed.ncbi.nlm.nih.gov/21030466/
- Vaiserman A, Krasnienkov D. Telomere Length as a Marker of Biological Age: State-of-the-Art, Open Issues, and Future Perspectives. Front Genet 2021;11:630186.
- Weindruch R, Walford R. The Retardation of Aging and Disease by Dietary Restriction. Choice Rev Online 1988;26(09):26-5101-26–5101.
- Piper MDW, Bartke A. Diet and aging. Cell Metab [Internet] 2008 [cited 2023 Aug 30];8(2):99–104. Available from: https://pubmed.ncbi.nlm.nih.gov/18680711/
- Baur JA, Pearson KJ, Price NL, Jamieson HA, Lerin C, Kalra A, et al. Resveratrol improves health and survival of mice on a high-calorie diet. Nat 2006 4447117 [Internet] 2006 [cited 2023 Aug 30];444(7117):337–42. Available from: https://www.nature.com/articles/nature05354
- Madeo F, Pietrocola F, Eisenberg T, Kroemer G. Caloric restriction mimetics: towards a molecular definition. Nat Rev Drug Discov 2014 1310 [Internet] 2014 [cited 2023 Aug 30];13(10):727–40. Available from: https://www.nature.com/articles/nrd4391
- Trepanowski JF, Kroeger CM, Barnosky A, Klempel MC, Bhutani S, Hoddy KK, et al. Effect of Alternate-Day Fasting on Weight Loss, Weight Maintenance, and Cardioprotection Among Metabolically Healthy Obese Adults: A Randomized Clinical Trial. JAMA Intern Med [Internet] 2017 [cited 2023 Aug 30];177(7):930–8. Available from: https://pubmed.ncbi.nlm.nih.gov/28459931/
- Bagherniya M, Butler AE, Barreto GE, Sahebkar A. The effect of fasting or calorie restriction on autophagy induction: A review of the literature. Ageing Res Rev [Internet] 2018 [cited 2023 Aug 30];47:183–97. Available from: https://pubmed.ncbi.nlm.nih.gov/30172870/
- Kujoth CC, Hiona A, Pugh TD, Someya S, Panzer K, Wohlgemuth SE, et al. Mitochondrial DNA mutations, oxidative stress, and apoptosis in mammalian aging. Science [Internet] 2005 [cited 2023 Aug 30];309(5733):481–4. Available from: https://pubmed.ncbi.nlm.nih.gov/16020738/
- Chistiakov DA, Sobenin IA, Revin V V., Orekhov AN, Bobryshev Y V. Mitochondrial aging and age-related dysfunction of mitochondria. Biomed Res Int [Internet] 2014 [cited 2023 Aug 30];2014. Available from: https://pubmed.ncbi.nlm.nih.gov/24818134/
- Li Q, Huang Y. Mitochondrial targeted strategies and their application for cancer and other diseases treatment. J Pharm Investig 2020 503 [Internet] 2020 [cited 2023 Aug 30];50(3):271–93. Available from: https://link.springer.com/article/10.1007/s40005-020-00481-0
- Sedlazeck FJ, Rescheneder P, Smolka M, Fang H, Nattestad M, Von Haeseler A, et al. Accurate detection of complex structural variations using single-molecule sequencing. Nat Methods 2018;15(6):461–8.
- Xu M, Palmer AK, Ding H, Weivoda MM, Pirtskhalava T, White TA, et al. Targeting senescent cells enhances adipogenesis and metabolic function in old age. Elife [Internet] 2015 [cited 2023 Aug 30];4(DECEMBER2015). Available from: https://pubmed.ncbi.nlm.nih.gov/26687007/
- McHugh D, Gil J. Senescence and aging: Causes, consequences, and therapeutic avenues. J Cell Biol [Internet] 2018 [cited 2023 Aug 30];217(1):65–77. Available from: https://pubmed.ncbi.nlm.nih.gov/29114066/
- Kirkland JL, Tchkonia T. Clinical strategies and animal models for developing senolytic agents. Exp Gerontol [Internet] 2015 [cited 2023 Aug 30];68:19–25. Available from: https://pubmed.ncbi.nlm.nih.gov/25446976/
- Fuhrmann-Stroissnigg H, Ling YY, Zhao J, McGowan SJ, Zhu Y, Brooks RW, et al. Identification of HSP90 inhibitors as a novel class of senolytics. Nat Commun [Internet] 2017 [cited 2023 Aug 30];8(1). Available from: https://pubmed.ncbi.nlm.nih.gov/28871086/
- Hernandez-Segura A, de Jong T V., Melov S, Guryev V, Campisi J, Demaria M. Unmasking Transcriptional Heterogeneity in Senescent Cells. Curr Biol [Internet] 2017 [cited 2023 Aug 30];27(17):2652-2660.e4. Available from: https://pubmed.ncbi.nlm.nih.gov/28844647/
- Tchkonia T, Zhu Y, Van Deursen J, Campisi J, Kirkland JL. Cellular senescence and the senescent secretory phenotype: therapeutic opportunities. J Clin Invest [Internet] 2013 [cited 2023 Aug 30];123(3):966–72. Available from: https://pubmed.ncbi.nlm.nih.gov/23454759/
- Campisi J, D’Adda Di Fagagna F. Cellular senescence: when bad things happen to good cells. Nat Rev Mol Cell Biol [Internet] 2007 [cited 2023 Aug 27];8(9):729–40. Available from: https://pubmed.ncbi.nlm.nih.gov/17667954/
- Coppé JP, Patil CK, Rodier F, Krtolica A, Beauséjour CM, Parrinello S, et al. A human-like senescence-associated secretory phenotype is conserved in mouse cells dependent on physiological oxygen. PLoS One [Internet] 2010 [cited 2023 Aug 30];5(2). Available from: https://pubmed.ncbi.nlm.nih.gov/20169192/
- Rodier F, Coppé JP, Patil CK, Hoeijmakers WAM, Muñoz DP, Raza SR, et al. Persistent DNA damage signalling triggers senescence-associated inflammatory cytokine secretion. Nat Cell Biol [Internet] 2009 [cited 2023 Aug 30];11(8):973–9. Available from: https://pubmed.ncbi.nlm.nih.gov/19597488/
- Krtolica A, Parrinello S, Lockett S, Desprez PY, Campisi J. Senescent fibroblasts promote epithelial cell growth and tumorigenesis: a link between cancer and aging. Proc Natl Acad Sci U S A [Internet] 2001 [cited 2023 Aug 30];98(21):12072–7. Available from: https://pubmed.ncbi.nlm.nih.gov/11593017/
- Baker DJ, Childs BG, Durik M, Wijers ME, Sieben CJ, Zhong J, et al. Naturally occurring p16Ink4a-positive cells shorten healthy lifespan. Nature 2016;530(7589):184–9.
- Farr JN, Xu M, Weivoda MM, Monroe DG, Fraser DG, Onken JL, et al. Targeting cellular senescence prevents age-related bone loss in mice. Nat Med [Internet] 2017 [cited 2023 Aug 30];23(9):1072–9. Available from: https://pubmed.ncbi.nlm.nih.gov/28825716/
- Zhu Y, Tchkonia T, Fuhrmann-Stroissnigg H, Dai HM, Ling YY, Stout MB, et al. Identification of a novel senolytic agent, navitoclax, targeting the Bcl-2 family of anti-apoptotic factors. Aging Cell [Internet] 2016 [cited 2023 Sep 4];15(3):428–35. Available from: https://pubmed.ncbi.nlm.nih.gov/26711051/
- Zhu Y, Tchkonia T, Pirtskhalava T, Gower AC, Ding H, Giorgadze N, et al. The Achilles’ heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell [Internet] 2015 [cited 2023 Sep 4];14(4):644–58. Available from: https://pubmed.ncbi.nlm.nih.gov/25754370/
- Van Deursen JM. The role of senescent cells in ageing. Nature [Internet] 2014 [cited 2023 Sep 4];509(7501):439–46. Available from: https://pubmed.ncbi.nlm.nih.gov/24848057/
- Kirkland JL, Tchkonia T. Clinical strategies and animal models for developing senolytic agents. Exp Gerontol [Internet] 2015 [cited 2023 Sep 4];68:19–25. Available from: https://pubmed.ncbi.nlm.nih.gov/25446976/
- Blackburn EH, Epel ES, Lin J. Human telomere biology: A contributory and interactive factor in aging, disease risks, and protection. Science [Internet] 2015 [cited 2023 Sep 5];350(6265):1193–8. Available from: https://pubmed.ncbi.nlm.nih.gov/26785477/
- Sanders JL, Newman AB. Telomere Length in Epidemiology: A Biomarker of Aging, Age-Related Disease, Both, or Neither? Epidemiol Rev [Internet] 2013 [cited 2023 Sep 5];35(1):112. Available from: /pmc/articles/PMC4707879/
- Blackburn EH. Structure and function of telomeres. Nature [Internet] 1991 [cited 2023 Sep 5];350(6319):569–73. Available from: https://europepmc.org/article/MED/1708110
- Olovnikov AM. A theory of marginotomy. The incomplete copying of template margin in enzymic synthesis of polynucleotides and biological significance of the phenomenon. J Theor Biol [Internet] 1973 [cited 2023 Sep 5];41(1):181–90. Available from: https://pubmed.ncbi.nlm.nih.gov/4754905/
- Harley CB, Futcher AB, Greider CW. Telomeres shorten during ageing of human fibroblasts. Nature [Internet] 1990 [cited 2023 Sep 5];345(6274):458–60. Available from: https://pubmed.ncbi.nlm.nih.gov/2342578/
- Lulkiewicz M, Bajsert J, Kopczynski P, Barczak W, Rubis B. Telomere length: how the length makes a difference. Mol Biol Rep [Internet] 2020 [cited 2023 Sep 5];47(9):7181–8. Available from: https://pubmed.ncbi.nlm.nih.gov/32876842/
- Martin H, Doumic M, Teixeira MT, Xu Z. Telomere shortening causes distinct cell division regimes during replicative senescence in Saccharomyces cerevisiae. Cell Biosci [Internet] 2021 [cited 2023 Sep 5];11(1):1–10. Available from: https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-021-00693-3
- Shay JW. Role of Telomeres and Telomerase in Aging and Cancer. Cancer Discov [Internet] 2016 [cited 2023 Sep 5];6(6):584–93. Available from: https://pubmed.ncbi.nlm.nih.gov/27029895/
- Aubert G, Lansdorp PM. Telomeres and aging. Physiol Rev [Internet] 2008 [cited 2023 Sep 5];88(2):557–79. Available from: https://pubmed.ncbi.nlm.nih.gov/18391173/
- Bernardes De Jesus B, Blasco MA. Aging by telomere loss can be reversed. Cell Stem Cell [Internet] 2011 [cited 2023 Sep 5];8(1):3–4. Available from: https://pubmed.ncbi.nlm.nih.gov/21211774/
- Kam MLW, Nguyen TTT, Ngeow JYY. Telomere biology disorders. npj Genomic Med 2021 61 [Internet] 2021 [cited 2023 Sep 5];6(1):1–13. Available from: https://www.nature.com/articles/s41525-021-00198-5
- Srinivas N, Rachakonda S, Kumar R. Telomeres and Telomere Length: A General Overview. Cancers (Basel) [Internet] 2020 [cited 2023 Sep 5];12(3). Available from: https://pubmed.ncbi.nlm.nih.gov/32121056/
- Armanios M, Blackburn EH. The telomere syndromes. Nat Rev Genet [Internet] 2012 [cited 2023 Aug 27];13(10):693–704. Available from: https://pubmed.ncbi.nlm.nih.gov/22965356/
- Savage SA, Niewisch MR. Dyskeratosis Congenita and Related Telomere Biology Disorders. GeneReviews® [Internet] 2023 [cited 2023 Sep 5];Available from: https://www.ncbi.nlm.nih.gov/books/NBK22301/
- Walne AJ, Marrone A, Dokal I. Dyskeratosis congenita: a disorder of defective telomere maintenance? Int J Hematol [Internet] 2005 [cited 2023 Sep 5];82(3):184–9. Available from: https://pubmed.ncbi.nlm.nih.gov/16207588/
- Bernardes de Jesus B, Vera E, Schneeberger K, Tejera AM, Ayuso E, Bosch F, et al. Telomerase gene therapy in adult and old mice delays aging and increases longevity without increasing cancer. EMBO Mol Med [Internet] 2012 [cited 2023 Sep 5];4(8):691–704. Available from: https://pubmed.ncbi.nlm.nih.gov/22585399/
- Jafri MA, Ansari SA, Alqahtani MH, Shay JW. Roles of telomeres and telomerase in cancer, and advances in telomerase-targeted therapies. Genome Med [Internet] 2016 [cited 2023 Sep 5];8(1). Available from: https://pubmed.ncbi.nlm.nih.gov/27323951/
- Pal S, Tyler JK. Epigenetics and aging. Sci Adv [Internet] 2016 [cited 2023 Sep 7];2(7). Available from: https://pubmed.ncbi.nlm.nih.gov/27482540/
- D’Aquila P, Rose G, Bellizzi D, Passarino G. Epigenetics and aging. Maturitas 2013;74(2):130–6.
- Horvath S, Raj K. DNA methylation-based biomarkers and the epigenetic clock theory of ageing. Nat Rev Genet [Internet] 2018 [cited 2023 Sep 7];19(6):371–84. Available from: https://pubmed.ncbi.nlm.nih.gov/29643443/
- Maegawa S, Lu Y, Tahara T, Lee JT, Madzo J, Liang S, et al. Caloric restriction delays age-related methylation drift. Nat Commun [Internet] 2017 [cited 2023 Sep 7];8(1). Available from: https://pubmed.ncbi.nlm.nih.gov/28912502/
- Jones MJ, Goodman SJ, Kobor MS. DNA methylation and healthy human aging. Aging Cell [Internet] 2015 [cited 2023 Sep 7];14(6):924–32. Available from: https://pubmed.ncbi.nlm.nih.gov/25913071/
- Biterge B, Schneider R. Histone variants: key players of chromatin. Cell Tissue Res [Internet] 2014 [cited 2023 Sep 7];356(3):457–66. Available from: https://pubmed.ncbi.nlm.nih.gov/24781148/
- Bannister AJ, Falcão AM, Castelo-Branco G. Histone Modifications and Histone Variants in Pluripotency and Differentiation. Chromatin Regul Dyn 2017;35–64.
- Sen P, Shah PP, Nativio R, Berger SL. Epigenetic Mechanisms of Longevity and Aging. Cell [Internet] 2016 [cited 2023 Sep 7];166(4):822–39. Available from: https://pubmed.ncbi.nlm.nih.gov/27518561/
- Yadav B, Pal S, Rubstov Y, Goel A, Garg M, Pavlyukov M, et al. LncRNAs associated with glioblastoma: From transcriptional noise to novel regulators with a promising role in therapeutics. Mol Ther Nucleic Acids [Internet] 2021 [cited 2023 Sep 7];24:728. Available from: /pmc/articles/PMC8099481/
- Li Y, Guo D. Identification of Novel lncRNA Markers in Glioblastoma Multiforme and Their Clinical Significance: A Study Based on Multiple Sequencing Data. Onco Targets Ther [Internet] 2020 [cited 2023 Sep 7];13:1087–98. Available from: https://pubmed.ncbi.nlm.nih.gov/32099410/
- Panni S, Lovering RC, Porras P, Orchard S. Non-coding RNA regulatory networks. Biochim Biophys Acta – Gene Regul Mech 2020;1863(6):194417.
- Jung HJ, Suh Y. Circulating miRNAs in ageing and ageing-related diseases. J Genet Genomics [Internet] 2014 [cited 2023 Sep 7];41(9):465–72. Available from: https://pubmed.ncbi.nlm.nih.gov/25269672/
- Jazwinski SM, Kim S. Examination of the Dimensions of Biological Age. Front Genet [Internet] 2019 [cited 2023 Sep 7];10(MAR):263. Available from: /pmc/articles/PMC6445152/
- Yamanaka S. Pluripotent Stem Cell-Based Cell Therapy-Promise and Challenges. Cell Stem Cell [Internet] 2020 [cited 2023 Sep 7];27(4):523–31. Available from: https://pubmed.ncbi.nlm.nih.gov/33007237/
- David SS, O’Shea VL, Kundu S. Base-excision repair of oxidative DNA damage. Nature [Internet] 2007 [cited 2023 Sep 7];447(7147):941–50. Available from: https://www.researchgate.net/publication/6254860_David_SS_O’Shea_VL_Kundu_SBase-excision_repair_of_oxidative_DNA_damage_Nature_447941-950
- Ocampo A, Reddy P, Martinez-Redondo P, Platero-Luengo A, Hatanaka F, Hishida T, et al. In Vivo Amelioration of Age-Associated Hallmarks by Partial Reprogramming. Cell [Internet] 2016 [cited 2023 Sep 7];167(7):1719-1733.e12. Available from: https://pubmed.ncbi.nlm.nih.gov/27984723/
- Benayoun BA, Pollina EA, Brunet A. Epigenetic regulation of ageing: linking environmental inputs to genomic stability. Nat Rev Mol Cell Biol [Internet] 2015 [cited 2023 Aug 27];16(10):593–610. Available from: https://pubmed.ncbi.nlm.nih.gov/26373265/
- Duan R, Fu Q, Sun Y, Li Q. Epigenetic clock: A promising biomarker and practical tool in aging. Ageing Res Rev [Internet] 2022 [cited 2023 Sep 7];81. Available from: https://pubmed.ncbi.nlm.nih.gov/36206857/
- Simpson DJ, Chandra T. Epigenetic age prediction. Aging Cell [Internet] 2021 [cited 2023 Sep 7];20(9). Available from: https://pubmed.ncbi.nlm.nih.gov/34415665/
- Kaushik S, Cuervo AM. Proteostasis and aging. Nat Med [Internet] 2015 [cited 2023 Sep 17];21(12):1406–15. Available from: https://pubmed.ncbi.nlm.nih.gov/26646497/
- Powers ET, Morimoto RI, Dillin A, Kelly JW, Balch WE. Biological and chemical approaches to diseases of proteostasis deficiency. Annu Rev Biochem [Internet] 2009 [cited 2023 Sep 17];78:959–91. Available from: https://pubmed.ncbi.nlm.nih.gov/19298183/
- Ferreira JV, da Rosa Soares A, Pereira P. Cell Non-autonomous Proteostasis Regulation in Aging and Disease. Front Neurosci [Internet] 2022 [cited 2023 Sep 17];16. Available from: https://pubmed.ncbi.nlm.nih.gov/35757551/
- Klaips CL, Jayaraj GG, Hartl FU. Pathways of cellular proteostasis in aging and disease. J Cell Biol [Internet] 2018 [cited 2023 Sep 17];217(1):51–63. Available from: https://pubmed.ncbi.nlm.nih.gov/29127110/
- Kim YE, Hipp MS, Bracher A, Hayer-Hartl M, Ulrich Hartl F. Molecular chaperone functions in protein folding and proteostasis. Annu Rev Biochem [Internet] 2013 [cited 2023 Sep 17];82:323–55. Available from: https://pubmed.ncbi.nlm.nih.gov/23746257/
- Sämann J, Hegermann J, von Gromoff E, Eimer S, Baumeister R, Schmidt E. Caenorhabditits elegans LRK-1 and PINK-1 act antagonistically in stress response and neurite outgrowth. J Biol Chem [Internet] 2009 [cited 2023 Sep 17];284(24):16482–91. Available from: http://intl.jbc.org/cgi/content/full/284/24/16482
- Ciechanover A, Kwon YT. Protein quality control by molecular chaperones in neurodegeneration. Front Neurosci [Internet] 2017 [cited 2023 Sep 17];11(APR):185–185. Available from: https://europepmc.org/articles/PMC5382173
- Masrori P, Van Damme P. Amyotrophic lateral sclerosis: a clinical review. Eur J Neurol [Internet] 2020 [cited 2023 Sep 17];27(10):1918. Available from: /pmc/articles/PMC7540334/
- Amin A, Perera ND, Beart PM, Turner BJ, Shabanpoor F. Amyotrophic Lateral Sclerosis and Autophagy: Dysfunction and Therapeutic Targeting. Cells 2020, Vol 9, Page 2413 [Internet] 2020 [cited 2023 Sep 17];9(11):2413. Available from: https://www.mdpi.com/2073-4409/9/11/2413/htm
- Cuervo AM, Bergamini E, Brunk UT, Dröge W, Ffrench M, Terman A. Autophagy and aging: the importance of maintaining “clean” cells. Autophagy [Internet] 2005 [cited 2023 Sep 17];1(3):131–40. Available from: https://pubmed.ncbi.nlm.nih.gov/16874025/
- Ebrahimi-Fakhari D, Saidi LJ, Wahlster L. Molecular chaperones and protein folding as therapeutic targets in Parkinson’s disease and other synucleinopathies. Acta Neuropathol Commun [Internet] 2013 [cited 2023 Sep 17];1(1). Available from: https://pubmed.ncbi.nlm.nih.gov/24314025/
- Singh A, Kukreti R, Saso L, Kukreti S. Oxidative Stress: A Key Modulator in Neurodegenerative Diseases. Mol 2019, Vol 24, Page 1583 [Internet] 2019 [cited 2023 Sep 17];24(8):1583. Available from: https://www.mdpi.com/1420-3049/24/8/1583/htm
- Kim GH, Kim JE, Rhie SJ, Yoon S. The Role of Oxidative Stress in Neurodegenerative Diseases. Exp Neurobiol [Internet] 2015 [cited 2023 Sep 17];24(4):325–40. Available from: https://pubmed.ncbi.nlm.nih.gov/26713080/
- Singh J, Vyas A, Wang S, Prasad R, editors. Microbial Biotechnology: Basic Research and Applications. 2020 [cited 2023 Jul 25];Available from: http://link.springer.com/10.1007/978-981-15-2817-0
- Madeo F, Eisenberg T, Pietrocola F, Kroemer G. Spermidine in health and disease. Science [Internet] 2018 [cited 2023 Sep 17];359(6374). Available from: https://pubmed.ncbi.nlm.nih.gov/29371440/
- Mendillo ML, Santagata S, Koeva M, Bell GW, Hu R, Tamimi RM, et al. HSF1 drives a transcriptional program distinct from heat shock to support highly malignant human cancers. Cell [Internet] 2012 [cited 2023 Sep 17];150(3):549–62. Available from: https://pubmed.ncbi.nlm.nih.gov/22863008/
- Hipp MS, Kasturi P, Hartl FU. The proteostasis network and its decline in ageing. Nat Rev Mol Cell Biol 2019 207 [Internet] 2019 [cited 2023 Sep 17];20(7):421–35. Available from: https://www.nature.com/articles/s41580-019-0101-y
- Franceschi C, Bonafè M, Valensin S, Olivieri F, De Luca M, Ottaviani E, et al. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci [Internet] 2000 [cited 2023 Sep 17];908:244–54. Available from: https://pubmed.ncbi.nlm.nih.gov/10911963/
- Fulop T, Larbi A, Dupuis G, Page A Le, Frost EH, Cohen AA, et al. Immunosenescence and Inflamm-Aging As Two Sides of the Same Coin: Friends or Foes? Front Immunol [Internet] 2018 [cited 2023 Sep 17];8(JAN). Available from: https://pubmed.ncbi.nlm.nih.gov/29375577/
- Nikolich-Žugich J. The twilight of immunity: emerging concepts in aging of the immune system. Nat Immunol [Internet] 2018 [cited 2023 Sep 17];19(1):10–9. Available from: https://pubmed.ncbi.nlm.nih.gov/29242543/
- Coppé JP, Desprez PY, Krtolica A, Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression. Annu Rev Pathol [Internet] 2010 [cited 2023 Sep 17];5:99–118. Available from: https://pubmed.ncbi.nlm.nih.gov/20078217/
- Salminen A, Kauppinen A, Kaarniranta K. Emerging role of NF-κB signaling in the induction of senescence-associated secretory phenotype (SASP). Cell Signal [Internet] 2012 [cited 2023 Sep 17];24(4):835–45. Available from: https://pubmed.ncbi.nlm.nih.gov/22182507/
- Hotamisligil GS. Inflammation and metabolic disorders. Nature [Internet] 2006 [cited 2023 Sep 17];444(7121):860–7. Available from: https://pubmed.ncbi.nlm.nih.gov/17167474/
- Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A. Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat Rev Endocrinol [Internet] 2018 [cited 2023 Sep 17];14(10):576–90. Available from: https://pubmed.ncbi.nlm.nih.gov/30046148/
- Goronzy JJ, Weyand CM. Understanding immunosenescence to improve responses to vaccines. Nat Immunol [Internet] 2013 [cited 2023 Sep 19];14(5):428–36. Available from: https://pubmed.ncbi.nlm.nih.gov/23598398/
- Pawelec G, Gupta S. Editorial: Immunology of Aging. Front Immunol [Internet] 2019 [cited 2023 Sep 19];10(JULY). Available from: https://pubmed.ncbi.nlm.nih.gov/31354744/
- Fulop T, Witkowski JM, Pawelec G, Alan C, Larbi A. On the immunological theory of aging. Interdiscip Top Gerontol [Internet] 2014 [cited 2023 Sep 19];39:163–76. Available from: https://pubmed.ncbi.nlm.nih.gov/24862019/
- Goldberg EL, Dixit VD. Drivers of age-related inflammation and strategies for healthspan extension. Immunol Rev [Internet] 2015 [cited 2023 Sep 19];265(1):63–74. Available from: https://pubmed.ncbi.nlm.nih.gov/25879284/
- Gruver AL, Sempowski GD. Cytokines, leptin, and stress-induced thymic atrophy. J Leukoc Biol [Internet] 2008 [cited 2023 Sep 19];84(4):915–23. Available from: https://pubmed.ncbi.nlm.nih.gov/18495786/
- Deleidi M, Jäggle M, Rubino G. Immune aging, dysmetabolism, and inflammation in neurological diseases. Front Neurosci [Internet] 2015 [cited 2023 Sep 19];9(APR). Available from: https://pubmed.ncbi.nlm.nih.gov/26089771/
- Fontana L, Partridge L, Longo VD. Extending healthy life span–from yeast to humans. Science [Internet] 2010 [cited 2023 Sep 19];328(5976):321–6. Available from: https://pubmed.ncbi.nlm.nih.gov/20395504/
- López-Lluch G, Hunt N, Jones B, Zhu M, Jamieson H, Hilmer S, et al. Calorie restriction induces mitochondrial biogenesis and bioenergetic efficiency. Proc Natl Acad Sci U S A [Internet] 2006 [cited 2023 Sep 19];103(6):1768–73. Available from: https://pubmed.ncbi.nlm.nih.gov/16446459/
- López-Lluch G, Irusta PM, Navas P, de Cabo R. Mitochondrial biogenesis and healthy aging. Exp Gerontol 2008;43(9):813–9.
- López-Lluch G, Navas P. Calorie restriction as an intervention in ageing. J Physiol [Internet] 2016 [cited 2023 Sep 19];594(8):2043–60. Available from: https://onlinelibrary.wiley.com/doi/full/10.1113/JP270543
- Guarente L. Calorie restriction and sirtuins revisited. Genes Dev [Internet] 2013 [cited 2023 Sep 19];27(19):2072–85. Available from: https://pubmed.ncbi.nlm.nih.gov/24115767/
- Gano LB, Donato AJ, Pasha HM, Hearon CM, Sindler AL, Seals DR. The SIRT1 activator SRT1720 reverses vascular endothelial dysfunction, excessive superoxide production, and inflammation with aging in mice. Am J Physiol Heart Circ Physiol [Internet] 2014 [cited 2023 Sep 19];307(12):H1754–63. Available from: https://pubmed.ncbi.nlm.nih.gov/25326534/
- Salminen A, Hyttinen JMT, Kaarniranta K. AMP-activated protein kinase inhibits NF-κB signaling and inflammation: impact on healthspan and lifespan. J Mol Med (Berl) [Internet] 2011 [cited 2023 Sep 19];89(7):667–76. Available from: https://pubmed.ncbi.nlm.nih.gov/21431325/
- Viollet B, Guigas B, Leclerc J, Hébrard S, Lantier L, Mounier R, et al. AMP-activated protein kinase in the regulation of hepatic energy metabolism: from physiology to therapeutic perspectives. Acta Physiol (Oxf) [Internet] 2009 [cited 2023 Sep 19];196(1):81–98. Available from: https://pubmed.ncbi.nlm.nih.gov/19245656/
- Madeo F, Pietrocola F, Eisenberg T, Kroemer G. Caloric restriction mimetics: towards a molecular definition. Nat Rev Drug Discov [Internet] 2014 [cited 2023 Sep 19];13(10):727–40. Available from: https://pubmed.ncbi.nlm.nih.gov/25212602/
- Mattison JA, Colman RJ, Beasley TM, Allison DB, Kemnitz JW, Roth GS, et al. Caloric restriction improves health and survival of rhesus monkeys. Nat Commun [Internet] 2017 [cited 2023 Sep 19];8. Available from: https://pubmed.ncbi.nlm.nih.gov/28094793/
- Colman RJ, Anderson RM, Johnson SC, Kastman EK, Kosmatka KJ, Beasley TM, et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science [Internet] 2009 [cited 2023 Sep 19];325(5937):201–4. Available from: https://pubmed.ncbi.nlm.nih.gov/19590001/
- Kennedy BK, Berger SL, Brunet A, Campisi J, Cuervo AM, Epel ES, et al. Aging: a common driver of chronic diseases and a target for novel interventions. Cell [Internet] 2014 [cited 2023 Sep 19];159(4):709. Available from: /pmc/articles/PMC4852871/
- McCarthy MI, Abecasis GR, Cardon LR, Goldstein DB, Little J, Ioannidis JPA, et al. Genome-wide association studies for complex traits: consensus, uncertainty and challenges. Nat Rev Genet [Internet] 2008 [cited 2023 Sep 19];9(5):356–69. Available from: https://pubmed.ncbi.nlm.nih.gov/18398418/
- Armanios M, Blackburn EH. The telomere syndromes. Nat Rev Genet [Internet] 2012 [cited 2023 Sep 5];13(10):693–704. Available from: https://pubmed.ncbi.nlm.nih.gov/22965356/
- de Jesus BB, Schneeberger K, Vera E, Tejera A, Harley CB, Blasco MA. The telomerase activator TA-65 elongates short telomeres and increases health span of adult/old mice without increasing cancer incidence. Aging Cell [Internet] 2011 [cited 2023 Sep 19];10(4):604–21. Available from: https://pubmed.ncbi.nlm.nih.gov/21426483/
- Zsurka G, Peeva V, Kotlyar A, Kunz WS. Is There Still Any Role for Oxidative Stress in Mitochondrial DNA-Dependent Aging? Genes (Basel) [Internet] 2018 [cited 2023 Sep 19];9(4). Available from: /pmc/articles/PMC5924517/
- Ziada AS, Smith MSR, Côté HCF. Updating the Free Radical Theory of Aging. Front Cell Dev Biol 2020;8:575645.
- Gorbunova V, Seluanov A, Mao Z, Hine C. Changes in DNA repair during aging. Nucleic Acids Res [Internet] 2007 [cited 2023 Sep 19];35(22):7466–74. Available from: https://pubmed.ncbi.nlm.nih.gov/17913742/
- Maegawa S, Lu Y, Tahara T, Lee JT, Madzo J, Liang S, et al. Caloric restriction delays age-related methylation drift. Nat Commun [Internet] 2017 [cited 2023 Sep 19];8(1). Available from: https://pubmed.ncbi.nlm.nih.gov/28912502/
- Levine ME, Lu AT, Bennett DA, Horvath S. Epigenetic age of the pre-frontal cortex is associated with neuritic plaques, amyloid load, and Alzheimer’s disease related cognitive functioning. Aging (Albany NY) [Internet] 2015 [cited 2023 Sep 19];7(12):1198–211. Available from: https://pubmed.ncbi.nlm.nih.gov/26684672/
- Ocampo A, Reddy P, Martinez-Redondo P, Platero-Luengo A, Hatanaka F, Hishida T, et al. In Vivo Amelioration of Age-Associated Hallmarks by Partial Reprogramming. Cell [Internet] 2016 [cited 2023 Sep 19];167(7):1719-1733.e12. Available from: https://pubmed.ncbi.nlm.nih.gov/27984723/
- Bacalini MG, Friso S, Olivieri F, Pirazzini C, Giuliani C, Capri M, et al. Present and future of anti-ageing epigenetic diets. Mech Ageing Dev [Internet] 2014 [cited 2023 Sep 19];136–137:101–15. Available from: https://pubmed.ncbi.nlm.nih.gov/24388875/
- Johnson SC, Rabinovitch PS, Kaeberlein M. mTOR is a key modulator of ageing and age-related disease. Nature [Internet] 2013 [cited 2023 Sep 19];493(7432):338–45. Available from: https://pubmed.ncbi.nlm.nih.gov/23325216/
- Quach A, Levine ME, Tanaka T, Lu AT, Chen BH, Ferrucci L, et al. Epigenetic clock analysis of diet, exercise, education, and lifestyle factors. Aging (Albany NY) [Internet] 2017 [cited 2023 Sep 19];9(2):419–46. Available from: https://pubmed.ncbi.nlm.nih.gov/28198702/
- Pal S, Tyler JK. Epigenetics and aging. Sci Adv [Internet] 2016 [cited 2023 Sep 19];2(7). Available from: https://pubmed.ncbi.nlm.nih.gov/27482540/
- Rea SL, Wu D, Cypser JR, Vaupel JW, Johnson TE. A stress-sensitive reporter predicts longevity in isogenic populations of Caenorhabditis elegans. Nat Genet [Internet] 2005 [cited 2023 Sep 19];37(8):894–8. Available from: https://pubmed.ncbi.nlm.nih.gov/16041374/
- Karch CM, Cruchaga C, Goate AM. Alzheimer’s disease genetics: from the bench to the clinic. Neuron [Internet] 2014 [cited 2023 Sep 19];83(1):11–26. Available from: https://pubmed.ncbi.nlm.nih.gov/24991952/
- Field AE, Robertson NA, Wang T, Havas A, Ideker T, Adams PD. DNA Methylation Clocks in Aging: Categories, Causes, and Consequences. Mol Cell [Internet] 2018 [cited 2023 Sep 19];71(6):882–95. Available from: https://pubmed.ncbi.nlm.nih.gov/30241605/
- McVicker G, Gordon D, Davis C, Green P. Widespread genomic signatures of natural selection in hominid evolution. PLoS Genet [Internet] 2009 [cited 2023 Sep 19];5(5). Available from: https://pubmed.ncbi.nlm.nih.gov/19424416/
- Kilpinen H, Dermitzakis ET. Genetic and epigenetic contribution to complex traits. Hum Mol Genet [Internet] 2012 [cited 2023 Sep 19];21(R1). Available from: https://pubmed.ncbi.nlm.nih.gov/22976472/
- Kirkland JL, Tchkonia T. Clinical strategies and animal models for developing senolytic agents. Exp Gerontol [Internet] 2015 [cited 2023 Sep 19];68:19–25. Available from: https://pubmed.ncbi.nlm.nih.gov/25446976/
- Xu M, Pirtskhalava T, Farr JN, Weigand BM, Palmer AK, Weivoda MM, et al. Senolytics improve physical function and increase lifespan in old age. Nat Med [Internet] 2018 [cited 2023 Sep 19];24(8):1246–56. Available from: https://pubmed.ncbi.nlm.nih.gov/29988130/
- Tchkonia T, Zhu Y, Van Deursen J, Campisi J, Kirkland JL. Cellular senescence and the senescent secretory phenotype: therapeutic opportunities. J Clin Invest [Internet] 2013 [cited 2023 Sep 19];123(3):966–72. Available from: https://pubmed.ncbi.nlm.nih.gov/23454759/
- Coppé JP, Patil CK, Rodier F, Sun Y, Muñoz DP, Goldstein J, et al. Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol [Internet] 2008 [cited 2023 Sep 19];6(12). Available from: https://pubmed.ncbi.nlm.nih.gov/19053174/
- Baker DJ, Wijshake T, Tchkonia T, Lebrasseur NK, Childs BG, Van De Sluis B, et al. Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature [Internet] 2011 [cited 2023 Sep 19];479(7372):232–6. Available from: https://pubmed.ncbi.nlm.nih.gov/22048312/
- Campisi J. Aging, cellular senescence, and cancer. Annu Rev Physiol [Internet] 2013 [cited 2023 Sep 19];75:685–705. Available from: https://pubmed.ncbi.nlm.nih.gov/23140366/
- Kulkarni AS, Gubbi S, Barzilai N. Benefits of Metformin in Attenuating the Hallmarks of Aging. Cell Metab [Internet] 2020 [cited 2023 Sep 19];32(1):15–30. Available from: https://pubmed.ncbi.nlm.nih.gov/32333835/
- Oh J, Lee YD, Wagers AJ. Stem cell aging: mechanisms, regulators and therapeutic opportunities. Nat Med [Internet] 2014 [cited 2023 Sep 19];20(8):870–80. Available from: https://pubmed.ncbi.nlm.nih.gov/25100532/
- de Keizer PLJ. The Fountain of Youth by Targeting Senescent Cells? Trends Mol Med [Internet] 2017 [cited 2023 Sep 19];23(1):6–17. Available from: https://pubmed.ncbi.nlm.nih.gov/28041565/
- Piccoli C, Ria R, Scrima R, Cela O, D’Aprile A, Boffoli D, et al. Characterization of mitochondrial and extra-mitochondrial oxygen consuming reactions in human hematopoietic stem cells. Novel evidence of the occurrence of NAD(P)H oxidase activity. J Biol Chem [Internet] 2005 [cited 2023 Sep 19];280(28):26467–76. Available from: https://pubmed.ncbi.nlm.nih.gov/15883163/
- García-Prat L, Martínez-Vicente M, Perdiguero E, Ortet L, Rodríguez-Ubreva J, Rebollo E, et al. Autophagy maintains stemness by preventing senescence. Nature [Internet] 2016 [cited 2023 Sep 19];529(7584):37–42. Available from: https://pubmed.ncbi.nlm.nih.gov/26738589/
- Beerman I, Seita J, Inlay MA, Weissman IL, Rossi DJ. Quiescent hematopoietic stem cells accumulate DNA damage during aging that is repaired upon entry into cell cycle. Cell Stem Cell [Internet] 2014 [cited 2023 Sep 19];15(1):37–50. Available from: https://pubmed.ncbi.nlm.nih.gov/24813857/
- Florian MC, Klose M, Sacma M, Jablanovic J, Knudson L, Nattamai KJ, et al. Aging alters the epigenetic asymmetry of HSC division. PLoS Biol [Internet] 2018 [cited 2023 Sep 19];16(9). Available from: https://pubmed.ncbi.nlm.nih.gov/30235201/
- Plotkin LI, Weinstein RS, Parfitt AM, Roberson PK, Manolagas SC, Bellido T. Prevention of osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin. J Clin Invest [Internet] 1999 [cited 2023 Sep 19];104(10):1363–74. Available from: https://pubmed.ncbi.nlm.nih.gov/10562298/
- Chambers SM, Studer L. Cell fate plug and play: direct reprogramming and induced pluripotency. Cell [Internet] 2011 [cited 2023 Sep 19];145(6):827–30. Available from: https://pubmed.ncbi.nlm.nih.gov/21663788/
- Longo VD, Panda S. Fasting, Circadian Rhythms, and Time-Restricted Feeding in Healthy Lifespan. Cell Metab [Internet] 2016 [cited 2023 Sep 19];23(6):1048–59. Available from: https://pubmed.ncbi.nlm.nih.gov/27304506/
- Kennedy BK, Berger SL, Brunet A, Campisi J, Cuervo AM, Epel ES, et al. Geroscience: linking aging to chronic disease. Cell [Internet] 2014 [cited 2023 Sep 19];159(4):709–13. Available from: https://pubmed.ncbi.nlm.nih.gov/25417146/
- López-Otín C, Galluzzi L, Freije JMP, Madeo F, Kroemer G. Metabolic Control of Longevity. Cell [Internet] 2016 [cited 2023 Sep 19];166(4):802–21. Available from: https://pubmed.ncbi.nlm.nih.gov/27518560/
- Campisi J. Senescent cells, tumor suppression, and organismal aging: good citizens, bad neighbors. Cell [Internet] 2005 [cited 2023 Sep 19];120(4):513–22. Available from: https://pubmed.ncbi.nlm.nih.gov/15734683/
- Moskalev A, Chernyagina E, Kudryavtseva A, Shaposhnikov M. Geroprotectors: A Unified Concept and Screening Approaches. Aging Dis [Internet] 2017 [cited 2023 Sep 23];8(3):354. Available from: /pmc/articles/PMC5440114/
- Moqri M, Herzog C, Poganik JR, Biomarkers of Aging Consortium, Justice J, Belsky DW, et al. Biomarkers of aging for the identification and evaluation of longevity interventions. Cell [Internet] 2023 [cited 2023 Sep 23];186(18):3758–75. Available from: https://pubmed.ncbi.nlm.nih.gov/37657418/
- Nakamura M, Gao Y, Dominguez AA, Qi LS. CRISPR technologies for precise epigenome editing. Nat Cell Biol 2021 231 [Internet] 2021 [cited 2023 Sep 23];23(1):11–22. Available from: https://www.nature.com/articles/s41556-020-00620-7
- Li Y. Modern epigenetics methods in biological research. Methods [Internet] 2021 [cited 2023 Apr 16];187:104–13. Available from: https://pubmed.ncbi.nlm.nih.gov/32645449/
- Wang K, Liu H, Hu Q, Wang L, Liu J, Zheng Z, et al. Epigenetic regulation of aging: implications for interventions of aging and diseases. Signal Transduct Target Ther 2022 71 [Internet] 2022 [cited 2023 Sep 23];7(1):1–22. Available from: https://www.nature.com/articles/s41392-022-01211-8
- Madeo F, Eisenberg T, Pietrocola F, Kroemer G. Spermidine in health and disease. Science [Internet] 2018 [cited 2023 Sep 23];359(6374). Available from: https://pubmed.ncbi.nlm.nih.gov/29371440/
- Muñoz-Espín D, Serrano M. Cellular senescence: from physiology to pathology. Nat Rev Mol Cell Biol [Internet] 2014 [cited 2023 Sep 23];15(7):482–96. Available from: https://pubmed.ncbi.nlm.nih.gov/24954210/
- Burggren W, Chapman K, Keller BB, Monticino M, Torday JS. Interdisciplinarity in the Biological Sciences. Oxford Handb Interdiscip [Internet] 2017 [cited 2023 Aug 1];101–13. Available from: https://academic.oup.com/edited-volume/27968/chapter/211586105
- Agaoglu NB, Unal B, Akgun Dogan O, Kanev MO, Zolfagharian P, Ozemri Sag S, et al. Consistency of variant interpretations among bioinformaticians and clinical geneticists in hereditary cancer panels. Eur J Hum Genet 2022;30(3):378–83.
- Bredenoord AL, Dondorp W, Pennings G, De Wert G. Ethics of modifying the mitochondrial genome. J Med Ethics [Internet] 2011 [cited 2023 Sep 23];37(2):97–100. Available from: https://pubmed.ncbi.nlm.nih.gov/21071569/
- Knupsky AC, Caballero MS. Applying an Ethical Interdisciplinary, Collaborative Approach to the Scholarship of Teaching and Learning. 2022 [cited 2023 Sep 23];95–109. Available from: https://link.springer.com/chapter/10.1007/978-3-031-11810-4_7

This work is licensed under a Creative Commons Attribution 4.0 International License.






