How to Cite | Publication History | PlumX Article Matrix
Analgesic and antiinflammatory study of surfactant modified liposomes
P. Muthuprasanna1, K. Suriaprabha2*, T. srinivasa Rao1, Vidya Mandava1 and B. Sindhu1
1Department of pharmaceutics, Vels College of pharmacy, Chennai - 600 117 India.
2Department of Pharmaceutics, C.L. Baid Mehta College of Pharmacy, Thorappakkam, Chennai - 600 096 India.
Corresponding Author E-mail: suriaapril14@yahoo.com
ABSTRACT: Liposomes are microscopic structures consisting one or more concentric lipid bilayers surrounding aqueous compartment within which water soluble drugs can be entrapped.Tween80 plays a vital role by increasing the drug permeation into the stratum corneum. In the present study, modified liposomes were produced by incorporating surfactant - polysorbate80 (Tween 80) into the lipid bilayer. The liposomes exhibited a superior entrapment stability compared with that of surfactant free liposomes (i.e., liposomes prepared with lipids and cholesterol).The invivo studies were carried to determine the effect of various formulation such as negative control (NC) which is a plane corbopol gel, drug entrapped liposomes (L), marketed sample which is treated as positive control (PC) and surfactant modified liposomes (SL) in delivering the drug diclofenac sodium through the skin. The animals showed a very poor analgesic and anti inflammatory response when treated with negative control but showed an enhanced response when treated with positive control, liposomal gel and surfactant modified liposomal gel. Among these, the formulation –surfactant modified liposomal gel gave an improved response than the other two formulations.
KEYWORDS: Analgesic; antiinflammatory effect; liposomes
Download this article as:| Copy the following to cite this article: Muthuprasanna P, Suriaprabha K, Rao T. S, Mandava V, Sindhu B. Analgesic and antiinflammatory study of surfactant modified liposomes. Biosci Biotechnol Res Asia 2008;5(1) |
| Copy the following to cite this URL: Muthuprasanna P, Suriaprabha K, Rao T. S, Mandava V, Sindhu B. Analgesic and antiinflammatory study of surfactant modified liposomes. Biosci Biotechnol Res Asia 2008;5(1). Available from: https://www.biotech-asia.org/?p=6629 |
Introduction
Drugs are being administrated since ancient times to treat various ailments. Galenicals and powders were the initial dosage forms to deliver the drugs. Presently drugs are being delivered as tablets, pills, capsules, suppositories, ointments, liquid orals, creams and injectables. Even though these conventional drug delivery systems ensure a prompt release of drug, it necessary to administer these types of dosage forms several times a day to achieve as well as to maintain drug concentration within the therapeutically effective range .This results in significant fluctuation in the plasma drug concentration.
Liposomes are microscopic structures consisting of one or more concentric lipid baitlayers surrounding aqueous compartment within which water soluble drugs can be entrapped. Liposomes were discovered in the early 1960’s and subsequently studied as cell membrane models1. They have since gained recognisition in the field of drug delivery. The particle size of liposome ranges from 20nm to 10nm in diameter 2. Liposomes are colloidal, vesicular structures composed of one or more lipid bilayers surrounding equal numbers of aqueous compartments 3. Surfactants play a vital role in modifying the characteristics of liposomes .A defined change in formulation components affects the physical and chemical characteristics of cationic liposomes (Cols) carriers in many ways4 .Therefore , a great degree of control can be exercised over the structure by modifying the “Cols” with various materials, leading to new innovations for carrier improvement 5 . In a study, ultra deformable liposomes for oestradiol skin delivery were refined using Span80 and Tween80 as edge activators compared with sodium choate6. Vesicles containing phosphatidyl choline (PC) mixed with edge activators and oestradiol were also prepared7 . Surfactants were successfully used for the oral administration of poly (butylcynoacrylate) nanoparticulate delivery systems (PBCA-Ness), double coated with Tween80 and Poly(Ethylene)glycol(PEG) 20,000 for brain delivery of hexpeptide damaging , an anti-nociceptive peptide that does not cross blood brain barrier(BBB) by itself8. In the present study, modified liposomes were produced by incorporating a surfactant polysorbate80 (Tween80), into the lipid bilayer. The liposomes exhibited a superior entrapment stability compared with surfactant free liposomes (i.e., liposomes prepared with lipids and cholesterol).These results indicate that polysorbate80 can be used to produce stable liposome without changing the unique macrophage distribution of this drug delivery system.
Here in the making of liposomes, Tween 80 plays a vital role by performing the following activities. It acts as a promoter in the drug delivery by increasing the permeation of the drug into the stratum corneum9. It is used to improve the stability. It is used to optimize the tissue distribution and decrease the toxicity of liposomes. On usage of this Tween80, there will be decrease in diameter; as a result there will be an increase in stability. By using Tween80 it is possible to modulate the elastic properties and diffusional microenvironment of carbopol gel.
Materials and Methods
Preparation of modified liposomal gel
Phosphotidyl choline (lecithin) based liposomal formulation were modified using an animal fat (Capraaegagrus hircus) spheronized with cholesterol and Tween80 by reverse phase evaporation technique10. Size of liposomal formulation was made in the range of 200nm-300nm by probe sonicator for aiding dermal layer permeability. A model drug diclofenac sodium was entrapped in to this liposomal formulation during emulsification and were matrixed in a carbopol 934 translucent gel at the neutral pH 7. The gel gave increased stability for the formulation and provided an ease of application for the transdermal drug delivery.
(ii) Invivo studies
The invivo studies were carried to determine the effect of various formulation such as negative control (NC) which is a plane carbopol gel, drugs entrapped liposomes (L), Marketed sample which is treated as positive control (PC) and surfactant modified liposomes (SL) in delivering the drug diclofenac sodium through the skin.
(a) Analgesic Effect – Tail Flick Method11
All the animal experiments were carried after obtaining the approval from the institutional animal ethical committee. The animals were maintained under standard environmental conditions and were fed with standard pellet with water ad libitum. The analgesic effect of four different branded gels was studied on wurster rats by tail flick method using analgesiometer (INCO).Animals were divided in to four groups each contain 5 wurstar rats .The groups were framed based on the markings over the animal. They were H(head) , B (Body) ,T ( Tail) and E (Ear).They were selected for uniformity in weight ranging from (150-200 gm).Basal reaction time was recorded by placing the tip (last 1-2 cm) of the tail on radiant heat source. The tail withdrawal due to heat (Flicking response) was taken as the end point. Normally, rat withdraws tail within 2-3 secs. A cut off period of 15 secs was used to prevent damage to the tail .After conformation of normal behavior by the basal reaction time, the gel preparation was applied on the last 2 cm tip of the rat tail and stimulation was given by the heat source. Animals failing to give response within 15 secs were considered to show the maximum analgesic effect and the results were tabulated.
(b) Analgesic Effect – Eddys Hot plate Method11
Swiss albino Mice was weighed and appropriately numbered. The basal reaction time was observed by the hind path jumping response (which ever appears first) in animals, when placed on the hot plate maintained at constant temperature (550 C). Normally animal showed such response within 6-8 secs. A cut off period of 15 secs is observed to avoid damage to the paws. Diclofenac liposomal gel was applied to the animal paws and the reaction time of animals on the hot plate at different intervals of time after the drug application was observed .As the reaction time increases with diclofenac, 15 secs is taken as maximum analgesia and the animals were removed from the hot plate to avoid injury to the paws.
(c) Antiinflamatory Effect11
Swiss albino mice was weighed and appropriately numbered. Markings were made on both the hind paws (left and right) just beyond tibia – tarsal junction, so that every time the paw is dipped in mercury column up to the fixed rise in mercury column which was compared with their right hind limb counter part to ensure constant paw volume. The initial paw volume ( left and right ) of each rat was determined by mercury displacement method ( sphygmomanometer).Divide the animals in to 3 groups each comprising of 4 mice .To all the groups 0.1 ml of 0.01 % v/v formalin solution is injected intra dermally to create inflammation in the paw. One group is taken as control and the other 3 groups were given plain liposomal gel (Without drug), liposomal gel with the drug entrapped and marketed gel respectively in to their left paw. The degree of inflammation was determined using the mercury displacement method (sphygmomanometer) and the results were tabulated.
(iii) Invivo studies (Using Franz diffusion cell)12
Permeation of diclofenac drug from gels across freshly excised rat skin were determined using franz diffusion cell. Male swiss albino rats 6.8 weeks old, weighing 250-300gm were used to obtain freshly excised full thickness skin. Animal was sacrificed by spinal dislocation. Hair from the abdominal region was light clipped, by means of surgical scissors taking care not to damage the stratum corneum. Under running tap water excised skin was cleared off from the adhering subcutaneous tissue and visceral debris avoiding excessive stretching. Skin section so prepared were immediately used for in-vitro permeation. Gel formulation equivalent to 1mg of diclofenac drug was spread uniformly on the epidermal surface of the suitable cut skin section from the above procedure, mounted on a diffusion cell, made with a clinical glass tube with 20mm internal diameter and 100mm height. The skin membrane with the formulation was tied securely to end of the tube, the other end kept open to ambient conditions, which acts as a donor compartment. This was immersed 2cm below the surface of 50ml of tyrrode solution in 100ml beaker as receptor compartment. The receptor compartment was thermo stated at 370c and stirred magnetically at constant speed for a specified time intervals (5, 10, 20, 30, 40, 50,60mts). A 5ml of the receptor compartment was taken and diluted to 10ml using 7.4pH phosphate buffer and diclofenac content was estimated by measuring the absorbance at 277nm after each sampling 5ml of tyrrode solution was replaced in the receptor compartment.
Results
The results of analgesic effect of the formulation determined by Tail flick method and Eddy’s hot plate method were plotted in graph1 and 2. The animals showed a very poor analgesic response when treated with negative control but showed an enhanced analgesic response when treated with positive control, liposomal gel and surfactant modified liposomal gel and among these, the formulation – surfactant modified liposomal gel gave an improved response than the other two formulations. Similar effect was also found in the decrease of paw edema volume during determination of anti-inflammatory response of those formulations. Those anti-inflammatory responses were plotted in graph-3. Surfactant modified liposomal gel gave faster reduction of paw edema volume to normal volume than the other two formulations (positive control and negative control).The results of invitro release study was determined and plotted in graph-4
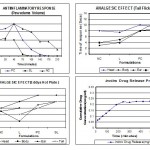 |
Graph 1
|
Discussion
The modified liposomal gel prepared by using Tween80 gave enhanced permeability and faster onset of action. The animal showed very poor analgesic response when treated with negative control but showed an enhanced analgesic response when treated with positive control, liposomal gel and surfactant modified liposomal gel. Among these, the formulation-surfactant modified liposomal gel gave an improved response than the other two formulations .Similar effect was also found in the decrease of paw edema volume during determination of anti-inflammatory response of those formulation.The surfactant included in the formulation aided the drug penetration which was entrapped inside the liposomal gel .The gel formed by the carbopol matrixed the liposomal formulation thus providing occlusive ness to the skin. The surfactant-Tween80 provided an easy penetration for the liposomes through the skin hastening the delivery of the drug to the systemic circulation. The carbopol helped the formulation to have an occlusive layer thus increasing the contact time for the liposome .The liposomes by its nature can easily penetrate the cells which further enhanced by the surfactant.
Conclusion
In conclusion, the surfactant modified liposome matrixed in carbopol gel made the drug to be delivered to the systemic circulation at a faster rate. Thus this surfactant modified liposomal gel can be a candidate for any other drug that has to be delivered to the systemic circulation. This can be exploited in designing any suitable drug delivery system towards the objective of enhanced drug delivery with reduced toxicity.
References
- Rawat M, Singh D, Saraf S, Saraf S., Lipid carriers: a versatile delivery vehicle for proteins and peptides, J Control Release.,128(2):269-80, ( 2008).
- Uner M, Yener G., Importance of solid lipid nanoparticles (SLN) in various administration routes and future perspectives.Int J Nanomedicine., 2(3):289-300, (2007).
- Samad A, Sultana Y, Aqil M., Liposomal drug delivery systems: an update review, Curr Drug Deliv., 4(4):297-305, (2007).
- Manosroi A, Thathang K, Werner RG, Schubert R, Manosroi J., Stability of luciferase plasmid entrapped in cationic bilayer vesicles. Int J Pharm., 5(2):221-226,(2006).
- Cortesi R, Marastoni M, Tomatis R, Menegatti E, Esposito E, Nastruzzi C.,Peptide-based cationic molecules for the production of positive charged liposomes and micelles.J Microencapsul.,25(2):71-81,( 2008).
- Garg M, Mishra D, Agashe H, Jain NK.,Ethinylestradiol-loaded ultraflexible liposomes: pharmacokinetics and pharmacodynamics. J Pharm Pharmacol., 58(4):459-68, (2006).
- Essa EA, Bonner MC, Barry BW.,Electrically assisted skin delivery of liposomal estradiol; phospholipid as damage retardant. J Control Release. 24;95(3):535-46, (2004).
- Li Y, Li JJ, Yu LC. Anti-nociceptive effect of neuropeptide Y in the nucleus accumbens of rats: an involvement of opioid receptors in the effect. Brain Res., 14; 940(1-2):69-78. (2002).
- Oh YK, Kim MY, Shin JY, Kim TW, Yun MO, Yang SJ, Choi SS, Jung WW, Kim JA, Choi HG., Skin permeation of retinol in Tween 20-based deformable liposomes: in-vitro evaluation in human skin and keratinocyte models., J Pharm Pharmacol.,58(2):161-6 ,( 2006).
- Fenske DB, Cullis PR., Liposomal nanomedicines.Expert Opin Drug Deliv. 5(1):25-44, (2008).
- Wang JR, Zhou H, Jiang ZH, Wong YF, Liu L.,In Vivo Anti-inflammatory and Analgesic Activities of a Purified Saponin Fraction Derived from the Root of Ilex pubescens., Biol Pharm Bull.,31(4):643-50,( 2008).
- Simonsen L, Fullerton A., Development of an in vitro skin permeation model simulating atopic dermatitis skin for the evaluation of dermatological products, Skin Pharmacol Physiol., 20(5):230-6, (2007).

This work is licensed under a Creative Commons Attribution 4.0 International License.





