How to Cite | Publication History | PlumX Article Matrix
Evans Blue Extravasation to Brain by Surfactant Modified Liposomes
Muthuprasanna1*, Manisha Mishra2 and K. Suriaprabha1
1Department of pharmaceutics, Hindu College of Pharmacy, Guntur India.
2CARISM, SASTRA, Tanjavur India.
Corresponding Author E-mail: p_ra2000@yahoo.com
ABSTRACT: Liposome are colloidal, vesicular structures capable of targeting to specific sites. Evans blue dye ( hydrophilic dye) were formulated in liposomes using phosphatidyl choline, cholesterol and those liposomes were modified using surfactants surfactants span 20 , span 40 , span 80 or tween 80 at various molar ratio and optimized for its stable vesicular formation. The particle size and FTIR analysis were performed for those formulations. Invivo studies were performed using those surfactant modified liposomes containing a biological marker - Evans blue dye to study the formulation penetrating power to brain. Span 80 and tween 80 combination of molar ratio 2:1 was efficient in modifying the liposomes towards delivering the dye to brain bypassing blood brain barrier than other surfactant modification of liposomes and the liposomes without surfactant. The result was further substantiated by carrying out SDS-PAGE gel electrophoresis using the brain homogenates, which showed visible bands of Evans blue dye for Span 80 tween 80 combinations indicating the targeting potential of surfactant modified liposomes to the brain. These results suggests that surfactants Span 80 tween 80 combination (molar ratio 2:1) used to modify liposomes proved to be the best carrier for desired drug to penetrate Blood brain barrier .
KEYWORDS: Liposome; Span 80; Tween 80; PAGE Gel Electrophoresis; Evans blue
Download this article as:| Copy the following to cite this article: Muthuprasanna, Mishra M, Suriaprabha K. Evans Blue Extravasation to Brain by Surfactant Modified Liposomes. Biosci Biotechnol Res Asia 2008;5(2) |
| Copy the following to cite this URL: Muthuprasanna, Mishra M, Suriaprabha K. Evans Blue Extravasation to Brain by Surfactant Modified Liposomes. Biosci Biotechnol Res Asia 2008;5(2). Available from: |
Introduction
New drug development is an expensive and incurs a great amount of time. The average cost for developing a new chemical entity is much more than the development of novel drug delivery System (NDDS). Such new chemical entity may take not less than ten years for their commercial use. But developing a novel drug delivery system is rather a no time consuming and an economic process and this NDDS development may take not more cost than the earlier new chemical entity .Thus it is wise to develop a suitable carrier for the existing drug molecule. This approach can significantly improve the drug performance towards patient compliance, safety and efficacy and can modeled to target the specific site 1.
Brain drug delivery is the rate limiting step in the translation of progress in the molecular neuroscience in to clinically effective neurotherapeutics for patience with disorders of the central nervous system (CNS). Progress in brain’s drug delivery has lagged behind other areas in the molecular neurosciences, because of the difficulties posed by the Blood Brain Barrier (BBB). Effective drugs have not been developed for most CNS disorders. Major small molecule drugs do not cross the BBB .Of over 7000 drugs in the comprehensive medicinal chemistry database only 5% of all drugs treat the CNS and these CNS active drugs only treat depression, schizophrenia and insomnia 2. The importance of developing effective neuropharmaceuticals and the lack of efficacy of existing strategies for drug delivery to brain emphasize the need to develop new approaches to drug transport across the BBB3. Colloidal carrier system is a promising strategy for improving drug delivery to the brain4. These system includes micro spheres, liposomes, lipid micro spheres, polymer micelles, nanoparticles, solid lipid nano particles, niosomes, vector mediated BBB transport etc 5. Nanotechnology is a break through technology expected to bring a revolutionary change in the field of life sciences including drug delivery, diagnostics, neutraceuticals and production of biomaterials6. Liposomes are the microscopic vesicles composed of one or more concentric lipid bilayers separated by water or aqueous buffer compartments with diameter ranging from 80 nm to 10 micron 7.
The lamellar vesicles are important as models for biomembranes, drug formulations, gene delivery and as vehicles for delivering various agents .Liposome can improve the therapeutic index and bioavailability, increase efficacy and reduce toxicity 8. Liposome can be used when an exiting formulation is not satisfactory and the drug offers superior therapeutic efficacy and safety over the existing formulation. These liposomal formulations have shown a significant increase in therapeutic efficacy and therapeutic indices in preclinical models than compared to their non liposomal formulation 9.
In our present study, we have investigated the ability of surfactant modified liposomes to transport Evans blue dye without any damage to brain cortex. We have examined the suitable surfactant and their optimized molar concentration that modifies the liposomes to penetrate BBB towards delivering the entrapped molecule.
Materials and Methods
Evans blue dye and Lecithin Soya were purchased from Himedia Laboratories Pvt. Ltd., India. Cholesterol and diethyl ether was obtained from Paxmy Speciality Chemicals, India. Span 20 and Tween 80 were purchased from Indian Research Products, India. Span 40 was obtained from Central Drug House (P) Ltd., Mumbai. Span 80 was purchased from NR Chem., Mumbai. All other ingredients used were of analytical grades. Rats (Wustar albino rat, male, 7 weeks old and approximately 150 gms body weight) were used for the study.
Formulation of Dopamine Hydrochloride
Liposome composed of Soya lecithin (Phosphotidyl Choline) and cholesterol were prepared with modification by reverse phase evaporation technique as described by Szoka and Papahadjoupoulos et al 10. Each Liposomal formulation was prepared by using Phospahatidyl choline and cholesterol with different surfactants such as span 20 (ES20), span 40 (ES40), span 80 (ES80) and span 80 and tween 80 combination (EST 80) and without surfactant (ENS) entrapping Evans blue dye (2% dye). In brief, Phosphotidyl choline, cholesterol at a molar ratio of 9:1were dissolved in diethyl ether. To this, Evans blue dye (2% w/v) in 5ml of a Phosphate Buffer Saline (PBS) of pH 7.4 were added along with surfactant span 20. The molar ratios for the surfactants were selected after optimizing based on their stability and vesicle formation. Then they were homogenized using a homogenizer (Tenbroeck tissue grinder – Kontes Glass Co., Vineland, NJ) for 20 minutes at 5000 RPM at 40 o C and then sonicated using a probe sonicator (Soniweild, India) for 5 minutes at 40 % frequency. This led to the formation of a reverse (w/o type) emulsion which later forms a semi solid gel like consistency. The residual diethyl ether solvent is evaporated further by using vacuum evaporator (BUCHI EL 131 Rotavapor, Germany) under reduced pressure (260 – 400 mm Hg) at 600 C. The lipid gel so formed was collapsed and transformed in to a fluid consistency by continuous vigorous mechanical agitation using a vortex mixer (REAX top, Heidolph Instruments GmbH & Co., Schwabach, Germany) .To this 5 ml of warm PBS (pH 7.4) was added to hydrate the vesicles thus producing suspension of liposomes. This formulation is designated as ES20. Similarly, other surfactants span 40, span 80 at molar concentration of 1:1(Lipid: surfactant) and span 80 with tween 80 combination at a molar concentration of 1:2:1(Lipid: span 80: tween 80) were prepared and designated as ES40, ES80 and EST80respectively. Without surfactant (ENS) liposomes were prepared by the same procedure but non inclusive of any surfactants.
Particle size analysis
Particle size of evans blue dye surfactant modified liposomal formulations (ES20, ES40, ES80, EST80 and ENS) was determined by optical microscopy (Olympus BH – 2 microscope) in which the eye piece micrometer were calibrated by laser ruled stage micrometer .A 500 microlitre of dispersion was placed on a microscopy glass slide below the objective of the microscope and was spread evenly over the slide. They were left to equilibrate until the particles slow down their visible movements and a cover slip was placed over the sample. Then particle counts of 100 numbers for its size were determined for each formulation under 10 X magnification. Values are expressed as standard error mean from the duplicate samples that were tested alongside of particle size analysis with sample size n=6. Significance of differences: P < 0.05 calculated using student’s t test.
Brain harvest and preparation
Wurstar albino rats used in this study were housed in a temperature of 23 + 20 C and light-controlled (12-h light/dark cycle) room with free access to water and food. All procedures were approved by our Institutional Ethics Committee and are in accordance with NIH Animal Care Guidelines. The Evans blue dye (1.5 ml, 2% dye) containing formulations (ES20, ES40, ES80, EST80 and ENS) were injected intraperitoneally to rats. After 30 minutes, rats were then anaesthetized by intraperitoneal administration of 10 mg /100 g ketamine (Ketanest, parke Davis, berlin, Germany) and then killed by cervical dislocation after 45 minutes of the administration. The brain was surgically harvested and examined for neuropathology. The brain was thoroughly washed with PBS and the Cerebral part were dissected into three equal portions through cerebral cortex as nearly as possible perpendicular to the longitudinal axis of the cerebral hemisphere . One portion was subjected for brain microtome slicing and another part of the brain was placed in formamide for 72 hours (Sigma, St Louis, MO) for histopathological studies. The third portion was stored in phosphate buffer pH 7.4, which was later homogenized and used for SDS-PAGE gel electrophoresis.
Microtomized brain slicing
The brain tissues were mechanically and biochemically stabilized in a fixative – neutral buffered formalin (10% formaldehyde in phosphate buffered saline (PBS)). The samples were immersed in multiple baths of progressively more concentrated ethanol to dehydrate the tissue, followed by a clearing agent – xylene and finally hot molten paraffin wax (impregnation). During this 12 to 16 hour process, paraffin wax replaces the xylene. Soft, moist tissues are turned into a hard paraffin block, which is then placed in a mold containing more molten wax (embedded) and allowed to cool and harden. The tissue is then sectioned into very thin (5 micrometer) sections using a rotary microtome (Leica RM2145) and are placed on a glass slide. These slices were then viewed under a microscope of magnification 10 X and 40 X (Olympus BH – 2 microscopes).
Histopathological studies
The cerebral cortex part for histopathological study was used .The brain tissues were fixed using – neutral buffered formalin (10% formaldehyde in phosphate buffered saline (PBS)). The samples were immersed in multiple baths of ethanol in ascending concentrations such as 0 %, 40%, 60%, 80 %, 90%, 96 %, and 3 times 100% for 1 hr in each step to dehydrate the tissue, followed by a clearing agent xylene and finally hot molten paraffin wax (impregnation). During this 12 to 16 hour process, paraffin wax replaces the xylene. Soft, moist tissues are turned into a hard paraffin block, which is then placed in a mold containing more molten wax (embedded) and allowed to cool and harden. The blocks embedded in paraffin were trimmed with a razor blade leaving a margin of about 1 mm of paraffin around the block and was trimmed almost to the tissue, while about 3-5 mm of paraffin were left on the back side, for attachment to a thin wooden rod (8 mm in diameter and 12 mm long). This wooden rod was then tightened into the block holder of a rotary microtome (Leica RM2145). The tissue is then sectioned using the knife of rotary microtome at 5 µm and are placed on a glass slide using a soft artists brush for Hematoxylin and eosin staining. Hematoxylin colors nuclei blue and eosin colors the cytoplasm pink.
SDS –PAGE GEL electrophoresis
In order to determine further the presence of Evans blue dye in the brain, SDS –PAGE GEL electrophoresis procedure were adopted. This technique proves to be a very good technique in determining even very small quantity of the dye in the brain sample. The harvested brain sample in phosphate buffer pH 7.4 for SDS – PAGE GEL electrophoresis was taken and homogenized on ice using tissue homogenizer (Tenbroeck tissue grinder – Kontes Glass Co., Vineland, NJ). The homogenate was centrifuged at 6000 rpm under 40 C for 10 minutes .The supernatant was analyzed for Evans blue dye identification using SDS –PAGE GEL electrophoresis. The SDS –PAGE GEL was prepared as follows. The acrylic plates were fixed using clips. A 10% of running gel solution was prepared by mixing tris-SDS pH 8.8 buffers, monomer, Ammonium per Sulphate (APS) and TEMED. Using a pipette, this running solution was poured gently along the side of the gel tubes up to 6cm of the acrylic plate. A few drops of water were added over the solution to avoid meniscus formation. The solution was left to polymerize. After the completion of polymerization the overlying water was removed carefully. A 5% spacer gel solution was prepared by mixing tries-Sodium Dodecyl Sulphate (Tris – SDS) 6.8 buffer, monomer, APS and TEMED and poured gently along the sides of the gel tubes and the sample comb was inserted. After the spacer gel polymerized, the comb was carefully removed and the wells were washed using tank buffer – Tris Glycine electrode buffer and the wells were filled with this tank buffer. Sucrose (20 µg) was dissolved in 50 µl of sample. To 50 µl of sample, 50 µl of sample buffer and bromophenol blue indicator was mixed and incubated for 8-10min in boiling water bath. After incubation, the sample was cooled to room temperature. The electrophoresis tank (Vertical Slab Gel Electrophoresis (Mini model), (8X7) cm for 7 Samples-05-01, Genei, Bangalore, India) was filled with 50ml of tank buffer in the lower tank. The remaining space of the gel plate was filled with tank buffer and 50ml of tank buffer was filled in the upper tank. The samples were added to the spacer gel using micropipette carefully into the wells taking care to avoid mixing of samples to their respective combed space. They were set aside for one hour for stabilization. The electrophoresis tank was connected to power pack of the electrophoretic apparatus and the electrophoresis was run at 250C. The voltage was adjusted constantly at 100V. The power supply was turned off when the bromophenol blue comes to the lower end of the gel plate. After the completion of electrophoresis, the gel was carefully removed from the plates and incubated in 10% tricarboxylic acid (TCA) for 90min to fix the proteins and the gel was stored in 7% acetic acid.
Results
Particle size analysis
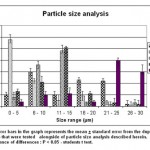 |
Graph 1
|
ES 40 formulations showed a wider distribution of particles in the size range of 0 – 5 µm (about 58 %) rather than other formulations but showed very less distribution in the size range of 6 -10 µm and more (Fig 1). It was very much less or negligible in the size range of 26 – 30 µm. But this was reverse in the case of non surfactant, as it showed very less size distribution in the size range of 0 – 5 µm but showed more prominence of its presence in size range greater than 21 µm. ES 20 showed greater size distribution within the size range of 6 – 10 µm but was very much minimal in 26 – 30 µm. In the case of ES 80 the maximum size was within the range of 11 – 15 µm but was very minimum in the size range of 21 – 25 µm. All showed an average presence in the size range of 6 – 10 micron. The EST 80 formulation had maximum of its vesicles in the size range of 11 – 15 µm but was minimal in the size range of 26 – 30 µm. S 80 rises its particle size from the range of 0 – 5 reaching peak at the range of 11 – 15 and abruptly falls to a very low size distribution in the range of above 15 micron.
Microtomized brain slicing
A macroscopically discernible blue area of dye extravasation was present on brain for the animal administered with EST 80 formulation. The blue staining was completely absent for the normal isolated brain (Fig 1). The basal part of the sliced cerebral cortex were more stained for the EST 80 ( TS ST 80) formulation when their 5 micron microtome sliced picture were seen , but staining were absent for the other formulation (Fig 2). This was clearly evident when observed under 40 X magnification (Fig 3). The slow invagination of Evans blue dye of EST 80 slowly through the peripheral brain parenchyma in to the interior brain cortex region could be clearly observed form the microtomized brain picture of TS ST 80 (EST 80) (Fig 3).
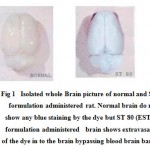 |
Figure 1: Isolated whole Brain picture of normal and ST 80 formulation administered rat. Normal brain do not show any blue staining by the dye but ST 80 (EST 80) formulation administered brain shows extravasation of the dye in to the brain bypassing blood brain barrier).
|
 |
Figure 2: T.S Microtomized section (5µm thickness) of isolated brain slices showing absence of evans blue dye in TS Normal (ENS) , TS S20 (ES20) , TS S40 (ES40) and TS S80 (ES80). But in the case of TS ST 80 (EST 80) extravasation of the Evans blue dye could be clearly observed.
|
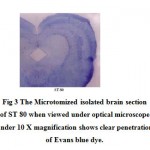 |
Figure 3: The Microtomized isolated brain section of ST 80 when viewed under optical microscope under 10 X magnification shows clear penetration of Evans blue dye.
|
Histopathological studies
Eosin – haematoxylin-counterstaining (blue) revealed distinct populations of stained cells with astrocytic morphology in the brain cortex for ST 80 formulation (Fig 4). These staining of cells were completely absent for other formulation. The Blue staining (Haematoxylin) for the nuclei and the pink (Eosin) for the cytoplasm were clearly visualized for all the formulation under 400 X magnification. But in the case of ST 80 formulation the brain parenchyma cells along with the eosin – haematoxylin staining showed blue large sized granular shaped structures which are a clear evident for the presence of Evans blue dye. These granular shaped dyes were completely absent or negligible in other formulations.
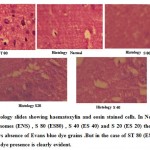 |
Figure 4: Histology slides showing haematoxylin and eosin stained cells. In Non surfactant Liposomes (ENS) , S 80 (ES80) , S 40 (ES 40) and S 20 (ES 20) the stained cells shows absence of Evans blue dye grains .But in the case of ST 80 (EST 80) Evans blue dye presence is clearly evident.
|
SDS –PAGE GEL electrophoresis
The gel photograph revealed the presence of prominent Evans blue dye band in the brain homogenate samples of ST-80 and control (0.1 %Evans blue 0.05µl). The blue dye band was prominent in the 10 % SDS gel under electrophoretic potential of 100 V and the position of the sample (ST 80) was inline with the control band. The other formulations brain homogenate failed to show any such kind of band (Fig 5).
 |
Figure 5: SDS PAGE Gel shows the presence of Evans blue dye (shown with an arrow) for ST 80 (EST 80) which is inline with pure Evans blue dye (ED) run at the same time on the same gel cast (shown with an arrow).
|
Discussions
The result of particle size distribution shows that S 40 surfactant was efficient enough to achieve more amounts of less particle sized liposomes within the size range of 0 – 5 micron which was superior to S80 surfactant. The liposomes in the absence of surfactant fails to achieve smaller size distribution on comparing to others and this proves that the emulsification using surfactant during the preparation is needed to achieve maximum reduction in the liposomal size and this reduced size has more potential in extravasating the blood capillaries towards targeting vital sites. Non surfactant modified liposomes mostly would form large unilamellar vesicles. Most of all the formulation showed an average population in the size range of 6 – 10 micron which proved to be the stable size in this manufacturing technique. The ST80 formulation showed a maximum population in the size range of 11 – 15 micron but falls down on either side proves that this formulation favors stability in this size range.
From the isolated brain pictures (Fig 1) it is clearly evident that the formulation EST80 was a very good carrier in carrying Evans blue dye to brain cortex thus staining the brain parenchyma. Further in the brain sliced picture (Fig 2) among the other formulation, the EST80 formulation was good enough to stain the brain which was further proved from the 40X magnification picture of the same which shows clear impregnation of the dye (Fig 3). The histopathological studies showed that there were no damage in the brain parenchyma due to these formulations but instead haematoxylin stained nuclei blue and eosin stained cytoplasm pink which were evident from those pictures. Among the other formulation, ES80 formulation histopathological picture showed the presence of blue colored dye grains but was absent in other formulations.SDS PAGE gel electrophoresis procedure provided a clear evidence (Fig 5) of presence of Evans blue dye by developing a blue band for ES80 formulation which is inline with the control – Evans blue dye itself ( showed by arrow marks ) .
The above results and discussion confers that the liposomes prepared by reverse phase evaporation technique and if modified with surfactant particularly span 80 and tween 80 at a molar concentration of 2:1 would make the entrapped liposomal drug extravasate through the brain capillaries and could achieve detectable presence in the brain parenchyma. More over those optimized liposomal formulation can have its particle size reduced to the need of targeting sites if above said surfactant combination used.
Conclusion
Thus the liposomes if modified using surfactant particularly span 80 and tween 80 at molar concentration of 2:1 could be a very good candidate to ferry the desired impermeable drug to brain without any pathological damage to the site. This formulation if developed further could also be a very good carrier for most of the neuropathological drugs which otherwise has access through intrathecal or implants or any other painful procedure. In conclusion, research work can further be initiated towards validating and standardizing this formulation for clinical and preclinical studies.
References
- Pardridge WM, Why is the global CNS pharmaceutical market so under – penetrated? Drug Disc Today ,7(1) :5 – 7,(2002).
- Ghose AK, Viswanandhan VN and Wendoloski JJ , A knowledge based approach in designing combinatorial or medicinal chemistry libraries for drug discovery .A quantitative and qualitative characterization of known drug databases , J Comb Chem , 1 : 55 – 68,(1999).
- Pardridge WM, Blood Brain Barrier and new approaches to brain drug delivery, the western journal of medicine, and 156 (3): 281 – 286, (1992).
- Suresh reddy j, Vobalaboina Venkateswarlu, Novel drug delivery systems for drug targeting to the brain, Drugs Fut, 29 (1):63 – 83,(2004).
- Joseph R Robinson and Vincent HL Lee, Ed. Controlled Drug Delivery Fundamentals and applications, 2nd Edn, Vol 29, Lippincott Williams’s publisher: 555 – 561, (1994).
- Bachhav D, Rao M, Madgulkar A and Rao S, Nanotecnology and blood brain barrier , Indian Drugs , 44 (4) : 245 – 251,(2007).
- Gregoriadis G, Engineering liposomes for drug delivery: progress and problems. Trends Biotechnol, 13 (12): 527 – 537, (1995).
- Drug Targeting System, Drug Delivery and Targeting for Pharmacists and pharmaceutical Scientists, Ed Anya M.Hillery and Andrew W Lloyd, Taylor and Francis Publication, USA, 1st Edn: 132 – 136, (2001).
- Tohoku J , Delivery of fungal beta galactosidase to rat brain by means of liposomes, Exp Med , 136 :219 – 229 (1982).
- Francis Szoka, Jr., and Demetrios Papahadjopoulos , Procedure For Preparation Of Liposomes With Large Internal Aqueous Space And High Capture By Reverse-Phase Evaporation , Proc. Natl. Acad. Sci. USA , Biochemistry, 75 (9): 4194-4198, (1978).
- Alfred martin and pilar bustamanle, Ed. Physical Pharmacy – Methods for determining particle size, 3rd edn, Lippincott Williams’s publisher, Philadelphia, Ed 2001, 430 – 431 (2001).
- Standard Operating Procedure , SOP for Use of Rotary Microtome , Dr Maria Sarris ed , Version 3.1 Aug 2004, University of south wales Publication, Edn 1st , Australia : 1 – 4 , (2004).
- Mayer’s hematoxylin solution , sigma aldrich publication , (procedure no. mhs) , revised 2003 – 09 ,AR – MED ltd , Runnymede malthouse egham ,TW 20 9BD ,UK : 1 – 3,( 2005).
- Manual For Studying Protein Expression Using 2-Dimensional Gel Electrophoresis (2DE) , Publication of Plant Breeding, Genetics and Biotechnology Division , International Rice Research Institute,1st edn :1 -20 , (2007).

This work is licensed under a Creative Commons Attribution 4.0 International License.





