How to Cite | Publication History | PlumX Article Matrix
Recent Advances in Hand Surgery and Future Prospects
N. Mariappan and M. Vignesh
Department of Hand Surgery, Sri Ramachandra Institute of Higher Education and Research, Porur, 600116 – Chennai, India.
Corresponding Author E-mail: drn_m@hotmail.com
DOI : http://dx.doi.org/10.13005/bbra/2738
ABSTRACT: The health care in hand surgery deals not only with surgical and non-surgical treatment and management. This field has been recognized much enough and development as independent clinical specialty. This review highlights the importance of hand surgery seems as a separate and independent clinical specialty, progress and challenges faced in past during its development, functional outcomes.
KEYWORDS: Clinical Specialty; Future Aspect; Hand Orthopedic; Hand Surgery; Microsurgical In Hand
Download this article as:| Copy the following to cite this article: Mariappan N, Vignesh M. Recent Advances in Hand Surgery and Future Prospects. Biosci Biotech Res Asia 2019;16(1). |
| Copy the following to cite this URL: Mariappan N, Vignesh M. Recent Advances in Hand Surgery and Future Prospects. Biosci Biotech Res Asia 2019;16(1). Available from: https://bit.ly/2IsJabL |
Introduction
The health care in hand surgery deal not only with surgical but also covers the non-surgical treatment and management of various problems arising in hand or upper extremity causing due to injury or infections.1 Hand surgery field utilizes and incorporates diverse techniques from orthopedics, General surgery, plastic surgery, vascular, neurosurgery and Micro vascular surgery and psychiatry. Unlike India, few western and Asian countries like Sweden, Finland and Singapore have recognized hand Surgery as a separate and independent clinical specialty, providing a four to six years hand surgery resident programs.
Scope of the Field
Hand surgery becomes entirely a new specialty as it requires specialist surgeons skilled with special techniques that are required to treat injuries and infections of the hand, which is at a crossroad between orthopedic, plastic and microsurgery. Supervision of fractures of the Hand and upper extremity, tendon repairs, tendon transfers, reconstruction following traumatic injuries, burn injuries to the Hand, correction of Hand deformities following rheumatoid and Hansen’s diseases, Volkmann’s ischemic contractures and congenital defects are some of the most common procedures performed.
Microsurgical reconstruction of amputated digits and limbs, repair and reconstruction of soft tissue and bone, nerve reconstruction, surgery for paralyzed upper limbs have shown a steady increase in the recent years. Sports and work place injuries are common following industrialization.2
History of Hand Surgery in the US
In United state during the World War II, major developments took place in hand surgery field,3 when the injured soldiers in battle field were besieged with numerous injuries particularly in their hands. At that point of time, the Dr. Norman T. Kirk a US army Surgeon, realized the need of dedicated specialized care center for those patients with injured hands and therefore played a key role in establishment of nine regional hand centers for treating wounded soldiers at army hospitals which also cater the training to surgeons. Dr. Sterling Bunnell, a consultant general surgeon of U.S. army dedicated his career in travelling between the military hand centers, with the purpose to educate hand surgeons. He was involved in the restoration and rehabilitation of 20,000 soldiers with injured hands in the wars. Dr. Bunnel further emphasized hand therapy as an essential part of the hand surgery management in hand troubles. This developments leads to generate first batch of 35 American surgeons at Bunnels’ teaching and the American Society for Surgery of the hand was found in 1947. The British Society for Surgery of the Hand (BSSH) was formed in 1956 with the aim to “promote and direct the development of Hand Surgery, to foster and co-ordinate education, study, and research in Hand surgery, and to disseminate knowledge of Hand Surgery among members of the medical and allied health professionals”.4
History of Hand Surgery in the India
In India, Surgery of the Hand trauma was a neglected one for a long time. It was to the credit of late Prof. C. Balakrishnan, who took up reconstructive surgery of the Hand trauma in a big way in fifties at Nagpur. Later, Dr. B.B. Joshi, an eminent orthopedic surgeon contributed to the care of injured Hands at Mumbai in Sixties. His Innovative works on Sensory flaps for finger-tip injuries has helped millions of Hands with sensate finger tips. Dr. Joshi formulated the need for post-operative splinting and physiotherapy in Hand Surgery for early return to work. He did a pioneering work on splints and Joshi External Stabilization system (JESS) is an example of his invention that has helped many injured Hands. Hand Club was formed in 1967 by The Indian Orthopedic Association.5
 |
Figure 1: Prof.C. Balakrishnan (left); Prof.B.B. Joshi (right).
|
The Indian Society for Surgery of the hand (ISSH) was founded on 15th August 1973 and the society held its first meeting in January 1974. Hand Injury Service, the first of its kind in our country was started in 1973 by Professor R.Venkataswamy at Stanley Medical College, Chennai. Professor G.Balakrishnan followed the good steps of Prof. R.Venkataswamy and he was instrumental in building an exclusive self-sufficient block for the Department. The department under Prof. G. Balakrishnan made tremendous strides and created a record for the maximum number of micro vascular procedures and surgeries for brachial plexus injuries.
 |
Figure 2: Prof.R. Venkataswamy(left); Prof.G. Balakrishnan(right).
|
There has been a steady flow of students and young surgeons to the department for training in Hand and microvascular surgery and the society at large has benefitted from the small candle lit by the Doyens of Hand surgery. 90% of pure Hand surgery patients were treated in day care basis and the rest admitted to an exclusive “Hand Injury Ward”. Rehabilitation Wing: Physiotherapy, occupational therapy and the splint making divisions were developed to cater to the needs of the patients with Hand injuries and Hand Surgeries. Training program: The program incorporates Undergraduates, interns, General and Orthopedic postgraduates. Physical Medicine and occupational therapy students also get a practical knowledge and lectures that are scheduled with regard to Hand and upper extremity problems.
Academic and Research Work
Oblique triangular flaps, Staged Neurovascular island flap of Prof RV and a bilobed groin flaps were described and effectively used for the benefit of the patients. A clinical entity called “thumb web burst” was identified and protocols for the management were formulated. A resting forearm splint for patients with groin flaps, and an active supinator splint, hand Immobilization by long aluminum splint for fractures was designed in the Department. Certified course for hand surgery was started and the Department was upgraded as an Institute by the initiative of Professor R.Venkataswamy. Yet another milestone in the field of hand surgery was the first bilateral hand transplant done in Tamil Nadu on 07/02/2018 at Stanley Medical College.
 |
Figure 3: Bilateral hand transplant in 29years/Male.
|
Microsurgery
Since the world’s first successful Replantation of the forearm in human in 1963 by Chen ZW in China, microsurgery has significant developments and many flaps are used with great success rate. The emphasis on replantation now is not on the success rate but on the functional outcome. In orthopedic reconstruction, microsurgery has a pivotal role in open fractures and osteomyelitis. The success rate of limb salvage in the treatment of sarcomas has steadily improved. With better understanding of the vascular anatomy and the technological advances in micro-surgery, ‘free-style’ free flap have been devised to meet the recipient need with decrease in donor site morbidity.6
 |
Figure 4: Reimplantation of Thumb.
|
Microsurgical transplantation of gratis like medial femoral condyle vascularized graft and/or revascularize an avascular scaphoid with fracture non-union and gratis vascularized fibula grafts aims to fill large bone defect in the upper and lower limbs are performed with great success. Super microsurgery for lymphedema of upper limbs with free vascularized lymph node transplantations will be a reality.
Recent Advances in Neural Repair and Regeneration for Hand Surgery
End-to-end stitch of nerves and autologous nerve grafts are considered ‘gold standard’ method to repair and reconstruction of peripheral nerves. Use of microsurgical technique and the understanding of the topographic anatomy of different nerves at different location are the keys to success.7,8
Suture Less Nerve Repair
Tissue glues or laser is utilized to carry out suture less nerve repair which prevents foreign-body inflammatory reaction and fibrosis. Fibrin glue is biocompatible, works faster and in principle easy to perform repairs which results in better axonal regeneration and fiber alignment.9
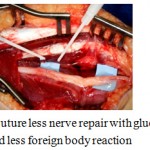 |
Figure 5: Suture less nerve repair with glue is simple, quicker and less foreign body reaction.
|
Laser-activated protein solders which contain bovine serum albumin was successfully used for suture less peripheral nerve repair with greater adhesion strength. Chitosan based adhesives require less temperature for activation and hence less tissue damage.10
End-to-Side Nerve Repair
When distal stump is unavailable, end to side repair of distal stump to an intact donor nerve helps to preserve function and prevents donor site morbidity.
Nerve Allografts and Xenografts
Nerve Allografts and Xenografts was sued as temporary scaffolding, diagonally which host axons regenerate. This avoids donor site morbidity. Immunosuppression with tacrolimus (FK 506) is used temporarily till allograft is replaced by host tissue.11
Nerve Conduits are channels for course of axonal sprouts starting from the proximal stump till the distal nerve stump and they allow diffusion of neurotrophic and neurotropic factors e.g. brain derived neurotrophic factor, nerve growth factor, and ciliary neurotrophic factor to improve the regeneration process. A variety of synthetic materials such as silicon, glycolide trimethylene carbonate, polyglycolic acid, polylactide-co-caprolone and biological materials like laminin, silk, collagen, autogenous vein/ muscle grafts have been used. Collagen conduits for nerve gaps up to 18mm in digital nerve repair in the hand of have shown good results.12
Molecular and Cell Therapy
Conduits seeded with cultured Schwann cells improves nerve rejuvenation. The utilization of fetal and adult progenitor neuronal cells and bone-marrow stem cells is a substitute to the use of Schwann cells.13
Brachial Plexus Injuries
Brachial plexus injury is a very difficult clinical problem and many methods of reconstruction including intra-plexal and extra-plexal nerve transfers and free functioning muscle transfers have improved the outcome. Investigation, nerve repair and grafting; nerve and tendon transfers for acute and chronic brachial plexus injuries are helpful. The support of an excellent occupational therapist is a boon for both children and adults with such injuries. Surgical management of Brachial plexus birth palsies include tendon releases, tendon transfers and de-rotation humeral osteotomies.14
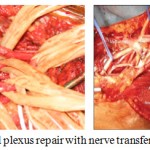 |
Figure 6: Brachial plexus repair with nerve transfer procedure.
|
Advances in Internal Fixation
Rigid fixation of fractures of the small bones of the Hand is a major advance in Hand surgery. The plates and screws made of stainless steel or Titanium are durable and compatible to the body. Bio-absorbable plates and screws are easy to use, have rigid fixation and there is no need for removal of implants. Injectable bone substitutes and calcium sulfate graft have great potential in treatment of fractures of distal radius. The main problem is to maintain the stability in osteoporotic or in comminuted fractures. Injectable calcium sulfate graft can be injected in liquid form through a small incision and is used to fill up defects in osteoporotic fractures enhances stability of the fixation.15
Burn Injuries to the Hand
The hands are concerned in close to 75-80% of all burns and the impending morbidity associated with hand burns can be extensive. Reconstructive surgery to improve the post burn deformities depends on the size of injury, meticulous surgical procedure, preoperative and postoperative hand treatment for the burned hand and is essential for a good functional outcome.16
Minimal invasive surgery: (1) Endoscopic carpal tunnel release (ECTR) was first introduced in 1989 by Okutsu and Chow.17 The advantages include: (1) Better scar; (2) Less palmar tenderness; and (3) Faster recovery with more rapid return of strength and resumption of work. Though the learning curve is greater the results are far superior. (ii). Scaphoid fractures: With routine use of CT for diagnosis and use of percutaneous cannulated screw fixation (PCSF) has achieved good bony union for stable fractures. The advantages include: (1) no prolonged plaster immobilization with better patient comfort; (2) good union rate and (3) Surgery performed under regional anesthesia.
Arthroscopy: (a) Wrist arthroscopy’s role is expanding in the treatment of wrist joint diseases. Triangular fibrocartilage injury and other ligamentous injuries of the wrist are common and can be managed with this technique. Arthroscopic assisted treatment of scapho-lunate instability, scaphoid nonunion and Kienbock’s disease gives good results. (b) Elbow arthroscopy: The results of Arthroscopic treatment of elbow synovitis, through small incisions are encouraging for persistent synovitis in rheumatoid arthritis despite adequate medical treatment with disease modifying agents. Persistent pain in osteoarthritis of the elbow can also be treated with arthroscopic techniques. Elbow arthroscopy is also useful in the management of intra-articular tumors and fractures. [18,19]
 |
Figure 7: An illustration of wrist arthroscopy.
|
Sports and Traumatic Injuries of the Wrist
Traumatic injuries caused in sports mainly in wrist and overuse syndromes afflicting the wrist are very common. The common injuries in ligamentous of the wrist include tears of the scapholunate ligaments and triangular fibrocartilage complex. Other than those bony injuries are next most common includes fractures of the distal radius and scaphoid.20 Dislocations concerning to the major articulations in wrist joint and intercarpal dislocations are less common. Depending on the sternness of injury, types of treatments range from occupational therapy, splinting to casting or even open type with minimally invasive surgical treatment.21 Wrist arthroscopy is used both as an adjunct for diagnosis and/or therapeutic management of the wrist in select ligamentous injuries. Chronic ligamentous volatility is corrected by ligament restoration surgery which resolves pain and restores function.
 |
Figure 8: Sports related Hand injuries are more common with contact sports.
|
Management of Spastic Conditions of the Upper Extremity
The most common causes of upper limb spasticity in adults are: Stroke, Spinal cord injury (SCI), Traumatic brain injury (TBI), Multiple sclerosis (MS), and Cerebral palsy (CP). Children with cerebral palsy tend to exhibit Diplegic, Quadriplegic or Hemiplegic pattern of spasticity. Management includes: (a) Splinting, Casting and Orthoses (b) Tizanidine, Diazepam, Dantrolene Sodium and (c) Chemo-denervation – neurolysis or neuromuscular blockade using Botulinum Toxin type A and Phenol. (d) Intrathecal baclofen (ITB) pump (e) Occupational Therapy and Physical Therapy Muscle over activity produces muscle shortening which increases spindle sensitivity. Rehabilitation and physical treatments are intended at augmentation of the overactive muscles are fundamental in management of spasticity.22
Management of Arthritis of the Base of the Thumb
Trapeziectomy offers excellent pain relief in patients in whom steroid injections are no longer effective.23 Recent surgical advances are: 1. Denervation Procedures: Dividing the nerves to painful joint result in significant pain relief is less invasive than trapeziectomy. The anatomy of the bones is preserved, movements are maintained, and the pain in thumb resolves. 2. Joint Replacement Surgery for the base of thumb gives very good outcomes with early return of movement and also maintains thumb strength.
Joint replacement: Arthroplasty of Wrist and hand (joint replacement) with artificial implants has replaced joint fusion (arthrodesis) and also allows preservation of motion. This enhances the utility of the pretentious hand, improving the quality of life for the patient. (I)Total elbow replacement: Total elbow replacement is technically demanding procedure used to treat advanced osteoarthritis or rheumatoid arthritis of the elbow joint (ii). Total wrist replacement: Recently, many new designs of total wrist Arthroplasty are developed. Screw fixation of the distal component decreases loosening of the prosthesis with promising results. (iii). Finger joint replacement: The prosthesis designs have improved with the available technology. Silicone finger joint replacement has been used to treat advanced finger joint arthritis of patients with rheumatoid arthritis.24
 |
Figure 9: A small joint prosthesis (Silicone).
|
Other New Developments: (A) Joint Instability
Reconstruction of the lax ligament end up with unfavorable results due to the unsatisfactory healing of ligamentous or tendon tissues to bone. Bone-ligament-bone graft has been applied in the treatment of joint instabilities in the hand and wrist. Bone- ligament-bone grafts from the distal radius were used to treat scapho-lunate instability with good results. A bone-ligament-bone graft harvested from the iliac crest can be used to reconstruct finger joint instabilities at the metacarpophalangeal, proximal interphalangeal and distal inter-phalangeal joints with very satisfactory results. (b). Tendon surgery should be simple and easy to apply. An improved technique of surgical repair of tendons and suture materials used enhance strength of the repair and allows early rehabilitation.25
Wide awake Hand surgery approach means the patient is not sedated for surgical procedures. Epinephrine decreases bleeding, hand surgery can be done without the need for a tourniquet and it is safe to inject in the human finger. It actively involves the patient to perform final adjustments of reconstructed tendons, joints and bones before the skin is closed.26,27 The mantra is “you can move your hand only as we instruct, but you must not use it”. Wide awake approach has also been supportive for Dupuytren’s contracture release, trapeziectomy, wrist arthroscopy and ulnar nerve decompression procedures.28
Advances in Physiotherapy
Effect of weightlessness on our body systems is a very recent in the field of physiotherapy. Ergonomics, sports physiotherapy and exercise rehabilitation are other exciting field of physiotherapy. Biomechanical analysis of human motion is measured in complicated gait laboratory using high-speed cameras, motion sensors, force plate, 3D motion analyzers, isokinetic dynamometers, pressure sensors, ultrasonography machine, pressure algometry to etc. The study of artificial limb, their training and exploring the scope and limits of these types of limbs for functional activity and sports is a great development. There has been integration of numerous new instruments like long wave diathermy (LWD), LASER, shock wave therapy and diagnostic ultrasound imaging in recent time.29,30
Recent Advances in Bioelectric Prostheses
There are 3 types of functional arm prostheses:
Body-powered: Allows only one degree of freedom at a time
Motorized: Driven by battery powered electric motor. Myoelectric prostheses and centrally controlled prostheses are subtypes that differ based on their control signals.
Hybrid: uses vision as an added sensor to control the prostheses.31
 |
Figure 10: Myoelectric prosthesis involve high technology and enables composite and complex hand movements.
|
A novel surgical intervention to improve myoelectric prosthetic control is targeted muscle reinnervation (TMR).32 This procedure involves reconnecting transected nerves to remaining muscles within the residual limb or chest. The newly innervated muscle is able to generate a unique myoelectric signal, which increases the overall number of sites of control and enhancing prosthetic function. These enervated muscles respond to neural input originally intended for hand or wrist actions, and hence the new sites of control are more intuitive for the user.
Organization of A Hand Injury Service
The following are the requirements for organization of a Hand Injury Service.
Outpatient care
Separate dressing areas for clean surgical cases and infected cases
Inpatient services
Postoperative care
Rehabilitation wing
Record keeping and statistician
Annual reports and auditing
Library and Educational Services
Medical Social Worker
Artist and Micro-photographer.
A 24 Hours Hand Injury Services with a dedicated operating room and an anesthesiologist will help the patients get immediate care under one roof. A Nursing staff will receive patients with exclusive Hand injuries and this reduces the routine emergency room delays. Anesthetist and staff must be posted exclusively for Hand injury Service for continuity of better care. A team of micro vascular surgeons will be on call in the event of receiving amputations that require replantation procedures. This will help ease the pressure of work on the surgeons taking care of other Hand Injuries. Hand injuries must be treated on an Emergency basis.
Working in dedicated Emergency OT should be simple and easy to man
Adequate number of instruments and materials must be available
Instrument packs must be ready with proper sterilization to avoid delays
Investigation facilities like X-rays of Hand and Biochemistry testing facilities
Constant interaction by the staff with the patients to cater their needs.
Future Prospects
Microsurgery
A 24-hour microsurgical service to be developed into a local referral centre for digital, hand and major limb replantation with success rates matching international standards is the ultimate aim of Hand Surgery Department. Telemanipulators, particularly in microsurgery, can progress surgical proposition by suppressing physiological tremor, thanks to movement demultiplication.
Robotics
Robotics have been developed which could be helpful for hand surgery. Passive robots are used for fluoroscopic navigation as an subsidiary for percutaneous screwing in the scaphoid bone tissue. In future, the robotic expertise potentially would become great technical resource with its easy-to-use, cheap, flawless prospect and which even allow remote-controlled surgery overseas.33,34
Hand Transplant Program
The Hand Transplant Program of the Louisville, Kentucky achieved the world’s foremost victorious hand transplant in January 1999.35 Hand and upper extremity transplantations are the common type of reconstructive transplantation performed most frequently. It is considered substitute to traditional prosthetics as standard treatment ensures optimal management throughout rehabilitation therapy.36,37 Current goals include Immunotherapy minimization or elimination, and insurance coverage to support this therapy.
Conclusion
The recent development of various new surgical specialties has led to advances in perfection of surgical techniques. The evolution of Hand surgery as a separate specialty will focus on reconstruction of hand and help the person earn his livelihood. In the long run, more young surgeons will be encouraged to take up Hand surgery and it will help improve the treatment protocols for those patients with Hand Injury in the near future.
References
- “About Hand Surgery”, American Society for Surgery of the Hand. Retrieved on 2011-02-24.
- George E. O. “Development of Hand Surgery”. The Journal of Hand Surgery. 2000;25A(4):616–628. doi:1053/jhsu. 2000.9752. PMID 10913201.
- American Society for Surgery of the Hand. The First Fifty Years. “The Second World War to 1971: The Founding. 1995;1-17. New York: Churchill Livingstone Inc. ISBN0-443-07761-4.
- Our History.British Society for Surgery of the Hand. Retrieved 25 July 2018.
- Rana R. E., Arora B. S. History of plastic surgery in India. J Postgrad Med [serial online] 2002;48:76. Available from: http://www. jpgmonline.com/text.asp?2002/48/1/76/144.
- Ono S., Sebastin S. J., Yazaki N., Hyakusoku H., Chung K. C. Clinical applications of perforator-based propeller flaps in upper limb soft tissue reconstruction. J Hand Surg Am. 2011;36:853-63.
CrossRef - Sunderland S. The intraneural topography of the radial, median and ulnar nerves. Brain. 1945;68:243–99.
CrossRef - Jabaley M. E., Wallace W. H., Heckler F. R. Internal topography of major nerves of the forearm and hand:a current view. J Hand Surg[Am]. 1980;5:1–18.
CrossRef - Wieken K., Angioi-Duprez K., Lim A., Marchal L and Merle M. Nerve anastomosis with glue: Comparative histologic study of fibrin and cyanoacrylate glue. J. Reconstr. Microsurg. 2003;19:17.
CrossRef - Lauto A., Hook J., Doran M., et al. Chitosan adhesive for laser tissue repair: in vitro characterization. Lasers Surg. Med. 2005;36:193–201.
CrossRef - Kvist M., Sondell M., Kanje M., Dahlin L. B. Regeneration in, and properties of, extracted peripheral nerve allografts and xenografts. J Plast Surg Hand Surg. 2011;45:122–128.
CrossRef - Trumble T. E & McCallister W. V. Repair of peripheral nerve defects in the upper extremity. Hand Clin. 2000;16:37-52.
- Frostick S. P & Kemp G. J. Schwann cells, neurotrophic factors and peripheral nerve regeneration. Microsurgery. 1998;18:397-405.
CrossRef - Giuffre L., Kakar S., Bishop A. T., Spinner R. J and Shin A. Y. “Current concepts of the treatment of adult brachial plexus injuries,” Journal of Hand Surgery A. 2010;35(4):678–688.
CrossRef - Chen Z., Liu H., Liu X., Lian X., Guo Z., Jiang H. J., et al. Improved workability of injectable calcium sulfate bone cement by regulation of self-setting properties. Materials Science and Engineering: C. 2013;33(3):1048-1053.
CrossRef - Howell J. W. Management of the Burned Hand in Burn Care and Rehabilitation: Principles and Practice. Richard RL, Staley MJ. Philadelphia, PA: FA Davis. 1994.
- Ichiro O.,Setsuo N., Yoshio T.,Yoshikazu U.”Endoscopic management of carpal tunnel syndrome”. Arthroscopy. 1989;5(1):11–8. doi:10.1016/0749-8063(89)90084-4. PMID 2706046.
CrossRef - Feldman M. D. Arthroscopic excision of type II capitellar fractures. Arthroscopy. 1997;13(6):743-8.
CrossRef - Micheli L. J., Luke A. C., Mintzer C. M. Elbow arthroscopy in the pediatric and adolescent population. Arthroscopy. 2001;17(7):694-9.
CrossRef - Osterman A. L., Terrill R. G. Arthroscopic treatment of TFCC lesions. Hand Clin. 1991;7:277–281.
- Gaston R. G., Loeffler B. J. Sports-specific injuries of the hand and wrist. Clin Sports Med. 2015;34:1–10.
CrossRef - Caldwell C. B., Braun R. M. Spasticity in the upper extremity. Clin Orthop 1974; 104: 80–91.
CrossRef - Swanson AB. Disabling arthritis at the base of the thumb: treatment by resection of the trapezium and flexible (sillicone) implant arthroplasty. J Bone Joint Surg [Am]. 1972;54:456–71.
CrossRef - Amadio P. C.,Shin A. Y. Arthrodesis and Arthroplasty of Small Joints of the Hand. In: Wolfe S. W., Hotchkiss R. N.,Pederson W. C.,Kozin S. H., editors. Green’s Operative Hand Surgery. 6th ed. Philadelphia, PA: Elsevier. 2011;390.
CrossRef - Kleinert H. E., Verdan C. Report of the committee on tendon injuries (International Federation of Societies for Surgery of the Hand). J Hand Surg (Am). 1983;8(5 Pt 2):794-8.
CrossRef - Lalonde D. H. Reconstruction of the hand with wide awake surgery. Clin Plast Surg. 2011;38(4):761-9. doi: 10.1016/j.cps.2011.07.005.
CrossRef - Lalonde D. H. Wide-awake flexor tendon repair. Plast Reconstr Sur;g. 2009;123(2):623-625.
CrossRef - Lavyne M. H., Bell W. O. Simple decompression and occasional microsurgical epineurolysis under local anesthesia as treatment for ulnar neuropathy at the elbow. Neurosurgery. 1982;11(1 Pt 1):6–11.
CrossRef - Baratto L., Calzà L., Capra R., Gallamini M., Giardino L., et al. Ultra-low-level laser therapy. Lasers Med Sci. 2011;26:103-112.
CrossRef - ZUBRyCKI I., GRANOSIK G. Using Integrated Vision Systems: Three Gears and Leap Motion, to Control a 3-finger Dexterous Gripper”, Recent Advances in Automation, Robotics and Measuring Techniques, Advances in Intelligent Systems and Computing. 2014;267:553-564.
- Bionic prosthetic hands: A review of present technology and future aspirations from: https://www.researchgate.net/publication/51759015_Bionic_prosthetic_hands_A_review_of_present_technology_and_future_aspirations.
- Huang H., Zhou P., Li G., Kuiken T. A. An analysis of EMG electrode configuration for targeted muscle reinnervation based neural machine interface. IEEE Trans Neural Syst Rehabil Eng. 2008;16(1):37-45.
CrossRef - Ballantyne G. H and Moll F. The daVinci Telerobotic Surgical System: The Virtual Operative Field and Telepresence Surgery. Surg Clin North Am. 2003;83(6):1293-304.
CrossRef - Allin S., Eckel E., Markham H., Brewer B. R. Recent trends in the development and evaluation of assistive robotic manipulation devices. Phys Med Rehabil Clin N Am. 2010;21:59e77.
- Breidenbach W. C., Gonzalez R., Kaufman C. L., Klapheke M. M., Tobin G. R., Gorantla V. S. Outcomes of the first 2 American hand transplants at 8 and 6 years post transplant. J Hand Surg [Am]. 2008;33(7);1037–47. [PMID: 18762094] DOI:10.1016/j.jhsa. 2008.02.015.
CrossRef - Roth E. S., Buck D. G., Gorantla V. S., Losee J. E., Foust D. E., Britton C. A. The role of imaging in patient selection, preoperative planning, and postoperative monitoring in human upper extremity allotransplantation. J Transplant. 2014;169546. http://doi.org/b42p.
- McDiarmid S. V., Azari K. K. Donor-related issues in hand transplantation.Hand Clin. 2011;27(4):545-52,x-xi. http://doi.org/d2tgj2.21.

This work is licensed under a Creative Commons Attribution 4.0 International License.





